Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
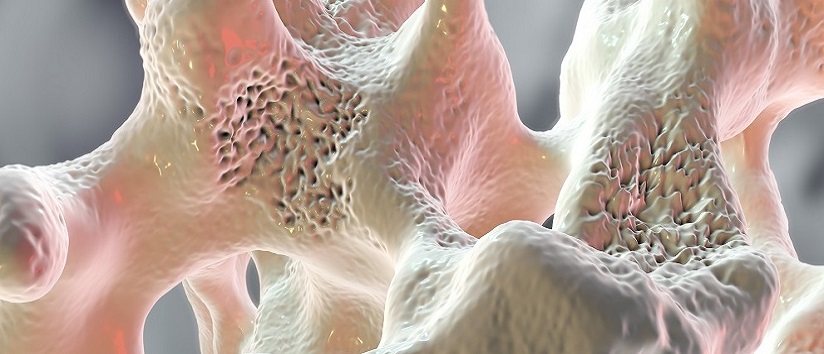
Boosting bone health
Practitioners can play a crucial role in helping patients to boost their bone health, and in raising awareness about bone conditions, the risks, the treatments and steps to prevention, reports Kathy Oxtoby.
---------------------------
This content is restricted to members of Pavilion Health Today. If you are an existing user, please log in. New users may register for free below.