Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Takotsubo cardiomyopathy (TCM) describes transient systolic and diastolic left ventricular dysfunction, most commonly following a physical or emotional event1 theorised to be the result of excessive catecholaminergic release.2 Here, we present a case report of a 90-year-old developing TCM following a fractured neck of femur (NOF).
Raised cardiac markers and an electrocardiogram (ECG) showing widespread ischaemic changes in multiple myocardial territories prompted an echocardiogram suggestive of TCM.
Although the systolic dysfunction in TCM recovers greatly within 2-6 weeks,3 this is too late for patients requiring urgent surgery for fractured NOFs, thus anaesthetic, orthopaedic and ortho-geriatric considerations are required to ensure optimal peri-operative care and subsequent recovery.
Case report
A 90-year-old lady presented to the emergency department with a painful hip following a fall. She had sustained a right sided comminuted inter-trochanteric femoral fracture which was shortened with posteromedial angulation. The mechanism of injury was described as a slip after showering with denial of preceding symptoms including chest pain and palpitations.
She was a non-housebound, mildly dependent individual with a medical history of osteoporosis, hypothyroidism, previous hypertension and a right hemicolectomy for an appendiceal mass. No further abnormality was detected on examination and she denied recent traumatic physical or emotional events preceding this injury.
The admission ECG was noted to have inferolateral T-wave inversion (II, III, AVF, V3-6), ST-elevation to V2-3 and left axis deviation (Figure 1a).
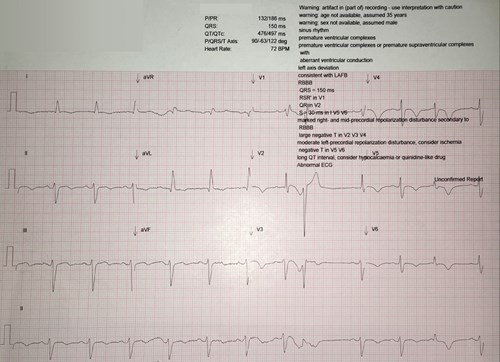
Acute coronary syndrome (ACS) was considered, thus troponin-I was added to admission bloods which was significantly raised (2352ng/l), decreasing to 1374ng/l when repeated 11 hours later. An echocardiogram (Figure 1b) the same day showed ballooning and akinesia of the left ventricular apex with preserved function in the mid and basal regions, with estimated ejection fraction of 45%. These findings were thought to be consistent with diagnosis of TCM. NT-ProBNP was mildly raised at 394.6ng/l.

After careful anaesthetic review, she was deemed stable for a short gamma nail insertion with cabling under general anaesthetic (GA) 36 hours after admission. Following this, she required transfer to the high dependency unit (HDU) for blood pressure support with metaraminol for 48 hours and transfusion of 2 units of red blood cells. Clopidogrel was commenced (due to aspirin intolerance) and low dose ramipril was initiated once her blood pressure was stable. Regular oxycodone and paracetamol was provided for analgesic purposes. She sustained no further complications and developed no clinical signs of heart failure. Further rehabilitation continued in a community hospital following a 25 day inpatient stay.
Discussion
Although systolic function tends to improve within 2-6 weeks of development of TCM,3 this is too late for patients with fractured NOFs. As congestive heart failure is a major pre-operative risk factor for early mortality following hip fracture,4 TCM is likely to be a significant risk factor too. Ortho-geriatricians, anaesthetists and orthopaedic surgeons should be aware of the implications that TCM may have for patients with emergency orthopaedic admissions.
In this case, urgent orthopaedic intervention was delayed for investigation of abnormal cardiac findings, anaesthetic review was extended for extra consideration of peri-operative complications, and 2 days of blood pressure support with metaraminol on HDU was required.
Attempts were made to reduce physiological stress with adequate analgesia, but consideration of regional anaesthesia, pre-operative anxiolysis and prophylactic beta-blockade have been suggested in such cases.5
Full assessment of TCM involves obtaining a coronary angiogram in the initial stages to rule out alternative pathology, as well as repeating an echocardiogram after a period of at least 4 weeks to ensure resolution of ventricular morphological changes.6 In this patient’s case, orthopaedic priority dictated initial investigations and the patient declined further follow up.
Key Points
- TCM can occur following physical trauma such as a fractured NOF.
- Admission ECGs are important in screening patients for TCM.
- Early cardiology input avoids incorrect diagnosis and unnecessary antiplatelet therapy pre-operatively.
- Avoiding stressors such as pain, GA and anxiety should be areas of focus.
Dr Angus Kitchin, Clinical Fellow, Musgrove Park Hospital
Dr Joanna Abramik, Speciality Registrar in Cardiology, Musgrove Park Hospital
Dr Prabhath Fernando, Consultant Geriatrician, Musgrove Park Hospital
Conflict of Interest: None.
Consent for Publication: Informed consent for publication of their clinical details and clinical images was obtained from the patient.
References
- Templin, C., Ghadri, J., Diekmann, J. et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med 2015; 373(10): 929-938.
- Wittstein, I., Thiemann, D., Lima, J., et al. Neurohumoral Features of Myocardial Stunning Due to Sudden Emotional Stress. N Engl J Med 2005; 352(6): 539-548.
- Lee, M. Time Course of Functional Recovery in Takotsubo (Stress) Cardiomyopathy: A Serial Speckle Tracking Echocardiography and Electrocardiography Study. J Cardiovasc Imaging 2020; 28(1): 50.
- Dodd, A., Bulka, C., Jahangir, A., et al. Predictors of 30-day mortality following hip/pelvis fractures. Orthop Traumatol-Sur 2016; 102(6): 707-710.
- Agarwal, S., Sanghvi, C., Odo, N., et al. Perioperative takotsubo cardiomyopathy: Implications for anesthesiologist. Ann Card Anaesth 2019; 22(3): 309.
- Ghurye, R., Price, D. Takotsubo Cardiomyopathy: An Abundance of Cases. GM 2018; 48(10).


