Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
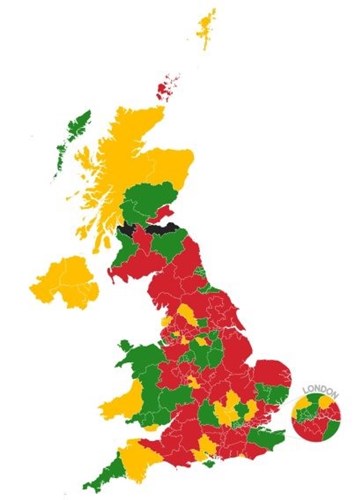
Only a quarter (26%) of areas in the UK have an effective pathway in place for the early detection of liver disease, according to new research by the British Liver Trust.
The research used a Freedom of Information request and found that the vast majority of areas in the UK (Figure 1) have little or no formal structures in place for detecting and managing liver disease and liver cancer. This is in sharp contrast to other chronic conditions such as diabetes and heart disease, where patients receive standardised care.
Three quarters of people in the UK are currently diagnosed when it is too late for effective intervention or treatment and one in four people diagnosed late in hospital sadly die within a couple of months.
The charity is now calling for urgent action to tackle these issues and is currently working with healthcare commissioners to encourage them to prioritise the earlier detection of liver disease and better patient care across all regions of the UK.
Early detection and prevention is key
Dr Helen Jarvis, Clinical Advisor for the British Liver Trust and lead author of the research, explains that although there are pockets of good practice, there are too many areas which do not have a consistent approach to testing and diagnosing which has led to thousands of avoidable deaths.
She continues: “The liver is an incredibly resilient organ, but only up to a point. Symptoms of liver disease often only appear once damage has progressed and the liver is starting to fail. However, 90% of liver disease is preventable and, in many cases, it’s reversible if caught in time. That’s why early detection and prevention are key.”
Hilary Todd had non-alcohol related fatty liver disease; she explains how the disease snuck up on her and led to her needing an urgent liver transplant in 2017. She said: “I hadn’t drunk alcohol for about 25 years and I thought I led a fairly healthy life until one day I suddenly felt very faint and vomited up a sink-full of blood. I was rushed to hospital and was later diagnosed with cirrhosis. It was too late for me to be effectively treated through lifestyle advice and I was told I needed a liver transplant.
“I will be forever grateful for all the wonderful doctors and nurses who cared for me and I know I am one of the lucky ones. However, my illness and the liver transplant could have been avoided if my condition had been picked up much earlier.”
“We need to take urgent action to stop this silent killer”
As deaths due to liver disease have more than doubled in the last 20 years and the condition is expected to soon overtake heart disease as the biggest cause of premature death in the UK, Pamela Healy OBE, Chief Executive of the British Liver Trust, said it is crucial that measures are taken now.
She said: “We need to take urgent action to stop this silent killer in its tracks. Although the results of our research are very concerning, we do know that there are areas of good practice and that the changes we’re calling for are entirely possible and will save many lives. We now need to take what’s working well in those areas with good liver patient care and apply them in others so that every person with liver disease gets the best possible care, no matter where in the UK they live.”


