Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
In December 2019 a cluster of cases of pneumonia of unknown cause was identified in Wuhan, the capital city of Hubei province of China. Scientists isolated a novel beta-coronavirus, which was designated severe acute respiratory syndrome coronavirus 2 (SARS-CoV2). The World Health Organization declared the disease caused by this virus as coronavirus disease 2019 (COVID-19) and a pandemic was declared in March 2020 1,2
Typical symptoms of Covid-19 include fever, dry cough and fatigue,3 however published reports also describe atypical and asymptomatic presentations.4,5
It is well-recognised in geriatric medicine that older, frailer, multi-morbid patients often present with atypical symptoms and the mortality rates in this age group are higher.6,7 The Royal Berkshire NHS Hospital (RBH) is a large district general hospital serving a population of approximately 600,000 residents, of whom approximately 20% are aged ≥65 years.8
This article aims to review the clinical characteristics of older patients diagnosed with Covid-19 in this hospital in March 2020 at the early stages of the pandemic and analyse the clinical course in this cohort of patients.
Key learning objectives:
- Clinical characteristics of older patients admitted with Covid-19
- Atypical symptoms of Covid-19 in older patients
- The correlation between Clinical Frailty Score and mortality rate from Covid-19
CPD credits: 0.5. Log them at myCPD
Method
This retrospective cohort study included all patients aged ≥65 years admitted to RBH who had a SARS-CoV2 positive test result on real-time reverse transcriptase-polymerase-chain reaction (RT-PCR) assay of nasal and pharyngeal swab specimen. Demographic, clinical, laboratory, treatment, and outcome data were obtained from Electronic Patient Record (EPR) and Connected Care.
Definitions
Fever was defined as a recorded temperature of at least 37·5°C. Lymphopenia was defined as a lymphocyte below the reference range used in the Trust (1.0-4.0 %).
Regarding comorbidities, cardiac history included those with ischaemic heart disease and cardiac failure due to any cause. Respiratory included those with progressive respiratory conditions such as chronic obstructive pulmonary disease and pulmonary fibrosis. End stage renal disease included only those receiving dialysis. Neurological conditions included previous stroke, Parkinson’s disease and multiple sclerosis. Active malignancy was the term used for patients with active haematological or solid organ tumours.
Results
106 patients tested positive for Covid-19 in March 2020 were aged ≥65 years, 10 were not admitted to RBH. We included 96 patients in the final analysis.
Age and sex
The median age was 82 years (ranging from 65 to 102) and 55 patients (57%) were male (table 1). Rates of infection were highest in males aged 85 to 89 years (n = 12), followed by males aged 80 to 84 years (n=11).
Table 1: Demographic, clinical and radiological findings of patients testing positive for Covid-19
| Demographics and clinical characteristics | Total
(n = 96) |
Survivor
(n = 54) |
Non-survivor
(n = 42) |
||
| Age (range) | 82 (65-102) | 83 (67-98) | 82 (65-102) | ||
| Sex | |||||
| Female | 41 (43%) | 24 (44%) | 17 (40%) | ||
| Male | 55 (57%) | 30 (55%) | 25 (60%) | ||
| Care home residents | 15 (16%) | 9 (17%) | 6 (14%) | ||
| Length of stay (mean) | 11.2 days | 12.7 days | 9.4 days | ||
| Smoking History | 30 (31%) | 13 (24%) | 17 (40%) | ||
| Medical Comorbidities | |||||
| Cardiac | 55 (57%) | 26 (48%) | 29 (69%) | ||
| Respiratory | 34 (54%) | 17 (31%) | 17 (40%) | ||
| Dementia | 24 (25%) | 14 (26%) | 10 (24%) | ||
| Diabetes | 18 (19%) | 9 (17%) | 9 (21%) | ||
| Neurological | 17 (18%) | 11 (20%) | 6 (14%) | ||
| Active malignancy | 18 (19%) | 9 (17%) | 9 (21%) | ||
| End stage renal failure | 3 (3%) | 2 (4%) | 1 (2%) | ||
| Chronic liver disease | 3 (3%) | 0 (0%) | 3 (7%) | ||
| Clinical Presentation | |||||
| Falls / Reduced mobility | 21 (22%) | 7 (13%) | 14 (33%) | ||
| Delirium | 42 (44%) | 21 (39%) | 21 (50%) | ||
| Fever | 50 (52%) | 28 (52%) | 22 (52%) | ||
| Cough | 47 (49%) | 30 (56%) | 17 (40%) | ||
| Hypoxia | 41 (43%) | 19 (35%) | 22 (52%) | ||
| Breathlessness | 55 (57%) | 30 (56%) | 25 (60%) | ||
| Gastrointestinal symptoms | 10 (10%) | 4 (4%) | 6 (14%) | ||
| Imaging Features | |||||
| Radiological changes on CXR or CT | 63 | 28 (52%) | 35 (83%) | ||
Clinical characteristics of patients with Covid-19
15 patients (16%) were admitted from a care home (table 1). The modal Clinical Frailty Score was 5.
At the time of presentation to hospital, 70 patients (73%) had typical symptoms (breathlessness, cough or lethargy) but during their clinical course slightly fewer (58 patients or 60%) had a fever. Of interest in our older population, common features of presentation also included delirium (42%) and falls or reduced mobility (18%). 10 patients had gastrointestinal symptoms at presentation and two of those had no “typical symptoms” during their clinical course. Four were asymptomatic at the time of having a positive Covid-19 swab specimen and one of those remained asymptomatic, whilst the remainder did subsequently develop typical symptoms such as cough and fever.
With regards to investigations, 79 patients (82%) were lymphopenic and many also had radiological changes (67%), of which four were CT scans and the remainder chest x-rays.
Comorbidities of patients with Covid-19
The most common comorbidities were chronic cardiac and respiratory conditions and dementia (57%, 39% and 27% respectively). Almost a third of patients had a smoking history and the mortality rate in this group was higher than in non-smokers (40% compared to 24%) (table 1).
The weight of the patient and the prescribing of ACE-inhibitor or angiotensin-2 receptor blockers had no effect on mortality.
Patient outcome after hospital stay with Covid-19
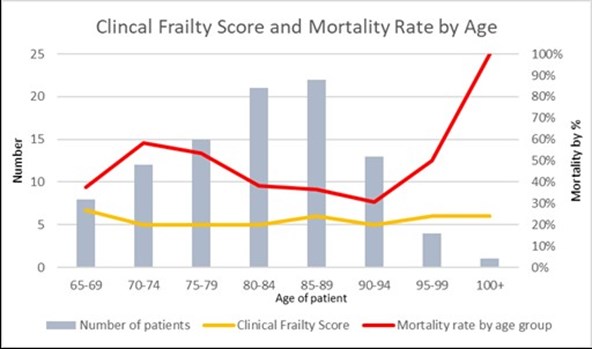
The average length of stay was 11 days (ranging from 1 to 44) and the mortality rate during that admission was 44%. The overall mortality rate was 44% and 60% of the mortalities were male. The highest rates of mortality were in those aged 70 to 74 years and those aged over 100 (58% and 100% respectively). The lowest mortality rates were those aged 65 to 69 years and 90 to 94 years (38% and 31% respectively).
Discussion
This retrospective cohort study identified that there were a high number of older males who contracted Covid-19 and were at higher risk of mortality than females of the same age groups. A significant number of the cohort had delirium as part of their clinical presentation. There appeared to be no correlation between Clinical Frailty Score and mortality rate (as seen in Figure 1).
The majority of the patients had ‘typical’ symptoms such as fever, cough and fatigue but delirium and reduced mobility were also common ‘atypical’ presentations of Covid-19 infection in our patient group. Lymphopenia and radiological changes were common but was not associated with increased risk of mortality.
A significant number had cardiac and respiratory comorbidities and the outcomes in these patients were poorer. There was also a higher mortality rate amongst smokers, in keeping with some current national data.9 Current hypothesis regarding obesity and use of ACE-inhibitors increasing mortality risk were not upheld in our patient group.
Our study had some limitations. Calculation of Clinical Frailty Score was performed on admission but the information informing this was limited and calculations often done by clinicians with limited experience of using the score before. Secondly, patient numbers at the extremes of age group were small, thus possibly skewing results.
Catherine Ashton, Specialist Registrar in Geriatrics and GIM , HETV
Ruhel Miah, Physician Associate , Elderly Care Medicine at Royal Berkshire Hospital
Nilangi Virgincar, Consultant Microbiologist, Royal Berkshire Hospital
Apurba Chatterjee, Consultant Physician Elderly Care Medicine, Royal Berkshire Hospital
References
- World Health Organization. Novel coronavirus (2019-nCoV) situation report-8. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200128-sitrep-8-ncov-cleared.pdf?sfvrsn=8b671ce5_2. January 28, 2020.
- World Health Organisation. Coronavirus disease (COVID-19) outbreak. https://www.who.int
- World Health Organization (WHO). Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) 2020 [cited 2020 1 March]. Available from: https://www.who.int/docs/default-source/coronaviruse/who-china-jointmission-on-covid-19-final-report.pdf
- Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ [Internet]. 2020 Apr 2 [cited 2020 Apr 5];369. Available from: https://www.bmj.com/content/369/bmj.m1375
- Shi F, Yu Q, Huang W, Tan C. 2019 Novel Coronavirus (COVID-19) Pneumonia with Hemoptysis as the Initial Symptom: CT and Clinical Features. Korean Journal of Radiology [Internet]. 2020 Feb 26 [cited 2020 Apr 5];21. Available from: https://doi.org/10.3348/kjr.2020.0181
- Hopkins C, Kumar N. Loss of sense of smell as marker of COVID-19 infection.pdf [Internet]. ENT UK. 2020 [cited 2020 Apr 5]. Available from: https://www.entuk.org/sites/default/files/files/Loss%20of%20sense%20of%2…
- British Geriatric Society. Atypical Covid-19 presentations in older people – the need for continued vigilance. Available from: https://www.bgs.org.uk/blog/atypical-covid-19-presentations-in-older-people-%E2%80%93-the-need-for-continued-vigilance
- Office for National Statistics. Deaths involving COVID-19, England and Wales: deaths occurring in March 2020. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19englandandwales/deathsoccurringinmarch2020
- Van Zyl-Smit R, Richards G, Leone F. Tobacco Smoking and COVID 19 Infection. Lancet Respir. Med. 2020 May 25. Available from: https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30239-3/fulltext#articleInformation


