Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
The novel coronavirus SARS-CoV-2 responsible for coronavirus disease 2019 (Covid-19) that emerged as a cluster of pneumonia cases in Wuhan, China in December 2019, shook the whole world by its highly contagious nature, virulence, and mortality. Within three months of the first reported case of the novel coronavirus, it had already been declared as a pandemic by the World Health Organization (WHO) in March 2020,1 resulting in an extensive wave of worldwide fear, lockdowns, and deaths.
While 80% of Covid-19 patients present with self-remitting mild respiratory illness, the minority that require hospitalisation has demonstrated high rates of mortality.1-5
Several studies have been published detailing the biochemical and haematological profile of SARS-CoV-2 infected patients. Lymphopenia and elevated inflammatory markers have been reported in hospitalised patients.6 One study found that 63% (26/41) of the patients who were admitted to a designated hospital in Wuhan with confirmed SARS-CoV-2 infection presented with low lymphocyte count.7 70.3% patients developed lymphopenia in a single-centre case series of 138 hospitalised patients in Wuhan, China. The degree of lymphopenia was significantly associated with a worse outcome.8
Additionally, advanced age has been linked with increased rates of fatality. Mortality approaching 8% among those aged 70 to 79 years and as high as 15% among adults older than 80 years have been reported by the Chinese Centre for Disease Control and Prevention.3 Similar findings have been reported from Italy, with mortality of around 12 and 20% among those aged 70 to 79 years and 80 years or older, respectively.9
Key learning objectives:
- Role of lymphopenia and elevated inflammatory markers in Covid-19
- Is lymphopenia a reliable marker for early diagnosis?
- Does lymphopenia have prognostic value in older patients?
CPD credits: 0.5. Log them at myCPD
Role of lymphopenia and elevated inflammatory markers in Covid-19
This study was designed to evaluate the clinical significance of lymphopenia as a diagnostic and prognostic marker of Covid-19 infection in older patients.
Materials and methods
A retrospective design was used to conduct this study at East Sussex Healthcare Trust’s Conquest hospital. Data was obtained from the registry of red-zone designated wards for Covid-19 cases. Based on the following inclusion criteria, a cohort of 38 patients was selected All the patients were above 75, admitted between March and April 2020, presented with symptoms of respiratory tract disease, and swabbed for SARS-CoV-2 RNA identification. Routine blood tests, such as full blood count (FBC), were performed.
Patients’ clinical laboratory data was retrospectively extracted from the electronic medical records. The findings were tabulated using Microsoft Excel spread sheet. The statistical analysis was performed using chi-squared test for categorical data, student’s t-test for continuous variables, and binomial regression for dichotomous variables. JASP statistical software was used in this study.
Results
The study cohort comprises of 38 patients. 19 of them tested positive for SARS-CoV-2 RNA, and 19 tested negative. The median age of our cohort was 91 years in the Covid-19 +ve group and 87 years in the Covid-19 -ve group. The most common comorbidities in Covid-19 +ve group were cardiovascular disease (62.3%), hypertension (52.6%), and obesity (36.8%). In the Covid-19 –ve group 52.63% of the patients has at least one cardiovascular disease, 36.84% hypertension, and 31.57% had Chronic Lung Disease.
Table 1. Summary of the epidemiological and haematological characteristics of the cohort
| Summary of patients characteristics | ||
| Parameter | Covid-19 positive
N = 19 |
Covid-19 negative
N = 19 |
| Sex | ||
| M
F |
11 (57.9%)
8 (42.1%) |
12 (63.2 %)
7 (36.8 %) |
| Age | ||
| Median
Range |
91
78 – 99 |
87
75 – 94 |
| White Cell Count | ||
| Low
Normal High |
2 (10.5%)
16 (84.2%) 1 (5.3%) |
0 (0%)
12 (63.2%) 7 (36.8%) |
| Lymphocytes on admission (× 10⁹ /L) | 0.85 (0.21 – 1.75) | 1.02 (0.23 – 2.26) |
| > 1.5
1 – 1.5 0.5 – 0.99 |
1 (5.3%)
7 (36.8%) 8 (42.1%) 3 (15.8%) |
2 (10.5%)
4 (21.1%) 11 (57.9%) 2 (10.5%) |
| Lymphocytes before admission | ||
| Normal
Low |
7 (36.8%)
12 (63.2 %) |
10 (52.6%)
9 (47.4%) |
| Outcome | ||
| Dead
Alive |
9 (47.4%)
10 (52.6%) |
2 (10.5%)
17 (89.5%) |
Haematological markers, including white cell count (WCC) and lymphocyte count, were evaluated on admission. In the Covid-19 +ve group 84.2% (n=16) had normal WCC, 10.5% (n=2) had leukopoenia (low WCC count), and 5.3% (n=1) leukocytosis (high WCC count).
On the other hand, in the Covid-19 –ve group, 63.1% (n=12) had normal WCC and 36.8% (n=7) had leukocytosis (high WCC count). 12 (63.2%) patients amongst the COVID-19 +ve group and 9 (47.4%) amongst the Covid-19-ve group were shown to have reduced lymphocyte count prior to admission. There was no statistical difference in the prevalence of lymphopenia between the two groups before admission (χ2 test, p = 0.328).
The degree of lymphopoenia, using absolute lymphocyte count, was also assessed on admission.The mean lymphocyte count was shown to be 0.85 x 109/L (range: 0.21 – 0.75) in the of Covid-19 +ve group and 1.02 x 109/L (range: 0.23 – 2.26) in the Covid-19 –ve. Statistical analysis using t-test for unpaired data demonstarted no significant difference in the absolute number of lymphocytes on admission between the two groups (p = 0.258).
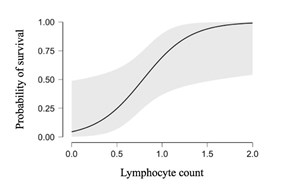
Mortality in Covid-19 +ve group was 47.4%, while 52.6% were discharged home. Binomial regression analysis showed that absolute lymphocyte count at the time of admission was an independent predictor of mortality (p
Discussion: clinical significance of lymphopenia
Since the outbreak of this on-going Covid-19 pandemic, many studies have been published to highlight the peculiar haematological characteristics of patients affected by the disease. Recent studies have shown an increased prevalence of low lymphocyte count in Covid-19 +ve patients,10 compared with the general population. However, when we retrospectively analysed the data of our elderly cohort, there was no statistical difference in the absolute lymphocyte count between the Covid-19 +ve and Covid-19-ve groups at the time of hospital admission.
Moreover, 63.2 % of patients in Covid-19 +ve and 47.4% in Covid-19 -ve group had lymphopoenia prior to admission. These facts suggest that lymphocyte count might not be a specific haematological marker of Covid-19 in the elderly population, and perhaps should not be used as a marker to request testing for Covid-19 diagnosis on admission. Advanced age is, in fact, a recognised factor in the development of immune response dysfunction affecting all lymphocytic lineages. Reduced lymphopoiesis, impaired antigen-specific immunity, tissue-specific changes are all characteristics features of ageing.1,5
Additionally, most patients in the Covid-19 +ve group who did not survive were shown to have marked degree of lymphopenia compared to those who survived. This demonstrates the prognostic value of lymphopenia at time of admission, which can be helpful in tailoring a prompt response for early interventions in Covid-19 disease patients. This has consistently been reported in several recently published studies, claiming that lymphopenia is a marker of severity and poor outcome in Covid-19 +ve patients.8
Since patients with Covid-19 disease present with a wide variety of symptoms, ranging from typical respiratory tract symptoms to atypical manifestations, we retrospectively analysed the level of WCC in our cohort of elderly patients. Surprisingly, a vast majority of Covid-19 +ve patients had normal WCC, which is contrary to the previously published data.5 This demonstrates that the atypical presentation of the disease in the older patients, poses a great challenge to the clinicians in making an early diagnosis of Covid-19.
Conclusion
Our study demonstrates that lymphopenia is not a specific marker in making an early diagnosis of Covid-19 in older patients (>75 years). Hence, its diagnostic value is limited in this age group. Based on the outcome of our study, we therefore propose that this haematological index should not be taken into consideration when evaluating the likelihood of infection in older patients.
However, it seems that the lymphocyte count is inversely related to in-hospital mortality, the lower the count the higher the mortality. Lymphopenia could be deemed a reliable predictor of mortality and could help clinicians identify patients with poor prognosis earlier on. Further studies with larger cohort are needed to better understand the disease in the older population
Limitations of the study
The retrospective nature of the study, relatively smaller sample size along with associated comorbidities in advanced age group of the cohort were some of the limiting factors while conducting the study.
Dr Muhammad Shahbaz, Senior House Office, Department of Health and Ageing, Conquest Hospital, East Sussex Healthcare Trust, St Leonards-on-Sea,
Dr Mariya Farooq. Core Medical Trainee Year 1, Department of Health and Ageing, Conquest Hospital, East Sussex Healthcare Trust, St Leonards-on-Sea,
Dr Gjulio Ciroi Tamos Marku, Foundation Year 1, Department of Health and Ageing, Conquest Hospital, East Sussex Healthcare Trust, St Leonards-on-Sea,
Dr. M.J.H. Rahmani, Consultant Physician. Department of Health and Ageing, Conquest Hospital, East Sussex Healthcare Trust, St Leonards-on-Sea
Conflict of interest: None
References
- WHO Director-General’s remarks at the media briefing on 2019-nCoV on 11 February 2020. (n.d.). Retrieved May 5, 2020, from https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020
- Channappanavar R, Fehr AR, Vijay R, et al. (2016). Dysregulated Type I Interferon and Inflammatory Monocyte-Macrophage Responses Cause Lethal Pneumonia in SARS-CoV-Infected Mice. Cell Host & Microbe, 19(2), 181–193. https://doi.org/10.1016/J.CHOM.2016.01.007
- Goyal P, Choi JJ, Pinheiro LC, et al. (2020). Clinical Characteristics of Covid-19 in New York City. The New England Journal of Medicine. https://doi.org/10.1056/NEJMc2010419
- Linton PJ, Dorshkind, K. (2004). Age-related changes in lymphocyte development and function. Nature Immunology, 5(2), 133–139. https://doi.org/10.1038/ni1033
- Montecino-RodriguezE , Berent-Maoz B, Dorshkind K. (2013). Causes, consequences, and reversal of immune system aging. The Journal of Clinical Investigation, 123(3), 958–965. https://doi.org/10.1172/JCI64096
- Xu,K, Chen, Y, Yuan J et al. (2020). Factors associated with prolonged viral RNA shedding in patients with COVID-19. Clinical Infectious Diseases. https://doi.org/10.1093/cid/ciaa351
- Huang C, Wang Y, Li X, et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 395(10223), 497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
- Wang D, Hu B, Hu C, et al. (2020). Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA, 323(11), 1061. https://doi.org/10.1001/jama.2020.1585
- Onder G, Rezza G, Brusaferro, S. (2020). Case-Fatality Rate and Characteristics of Patients Dying in Relation to COVID-19 in Italy. JAMA. https://doi.org/10.1001/jama.2020.4683
- Yun H, Sun Z, Wu J, et al. (2020). Laboratory data analysis of novel coronavirus (COVID-19) screening in 2510 patients. Clinica Chimica Acta, 507, 94–97. https://doi.org/10.1016/J.CCA.2020.04.018


