Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Depression is the most common mental health issue worldwide and affects around 22% of men and 28% of women over 65 years old,1 yet it is estimated that 85% of older people with depression receive no help at all from the NHS.1
Depression is a mental disorder that can have multiple presenting features in elderly, which may be more subtle than the traditional features. These include low mood, anhedonia, feelings of guilt, low self-worth, disturbed sleep/ appetite, low energy, and poor concentration.
Studies show that most older adults feel satisfied with their lives, despite having more illnesses or physical problems so it is a myth that depression is a normal part of ageing.2 However, important life changes may cause feelings of uneasiness, stress, and sadness. After a period of adjustment, many older adults can regain their emotional balance, but others do not and may develop depression.
Key learning objectives:
- How to diagnose depression in older patients
- Non-pharmacological management of depression
- Managing side effects of depression medications in the older age group
CPD credits: 0.5. Log them at myCPD
How to diagnose depression
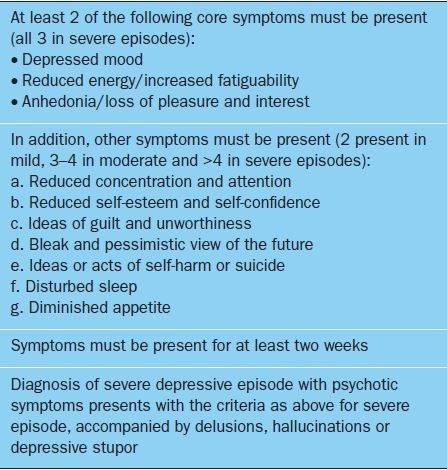
The diagnostic criteria for depression in the older patient are the similar to those in younger patients; In the UK, the World Health Organization ICD-10 diagnostic criteria are commonly used.3
Rating scales may be useful in determining severity and are recommended in NICE guidelines.5 Rating scales validated for use in the elderly (eg Patient Health Questionnaire 9 (PHQ-9), Geriatric Depression Scale, Hospital Anxiety and Depression Scale, Cornell Scale for Depression in Dementia) should ideally be used.
The bedrock of diagnosis is undoubtedly skilled clinical interview, mental state examination and good collateral history from relatives/carers. There are some important differences in the presentation of depression in old age. A meta-analysis found that although many of the principal symptoms were similar, older people are likely to demonstrate more agitation, hypochondriasis and somatic symptoms.6 Instead of explicitly complaining of depressed mood, elderly patients may describe more non-specific symptoms such as insomnia, anorexia or fatigue.
Comprehensive physical assessment is particularly important in older patients, both in terms of excluding underlying organic causes and identifying potential exacerbating factors. A number of chronic health problems have been shown to be associated with depression in later life, including stroke, Parkinson’s disease, cancer, heart disease, arthritis, COPD and endocrine disorders.
The Geriatric Depression Scale (GDS) is ideal in evaluating the clinical severity and monitoring treatment. It is easy to administer, needs no prior psychiatric knowledge and has been well validated in many environments.7 The 15-item (GDS-15) and 4-item (GDS-4) versions of the GDS are also both widely used. The systematic use of short GDS versions in Primary Care may increase detection rates of depression among the elderly, although shorter version is less useful in assessing the severity of the depressive episodes.8
Treatment of depression in older patients
Selection of antidepressant medication should be based on the side effect profile and the risk of drug-drug interaction. NICE recommends that selective serotonin reuptake inhibitors (SSRI) should normally be used as first-line treatment for depression in all age groups.5
Given the high rate of polypharmacy in the older patient, drug interactions are an important consideration. SSRIs such as citalopram and escitalopram (along with non-SSRIs mirtazapine and venlafaxine) have minimal effect on the cytochrome P450 system and so have a reduced risk of pharmacokinetic interactions. By contrast, fluoxetine and paroxetine are strong inhibitors of CYP2D6 while sertraline has a moderate inhibitory effect.9
It is important to be aware of the anticholinergic side-effects of SSRIs, which include postural hypotension and sedation, though these are less common with SSRIs than with tricyclic antidepressants (TCAs).10
Hyponatraemia is a potentially serious adverse effect and has been reported with almost all SSRIs in addition to the serotonin and noradrenaline reuptake inhibitor (SNRI) venlafaxine. When prescribing in at-risk groups, monitoring of urea and electrolytes can be useful, in addition to being vigilant for clinical features such as lethargy, muscle cramps, anorexia and headaches.
SSRIs are also associated with a modestly increased risk of upper GI tract bleeding in older people. NICE guidance recommend consideration should be given to co-prescribing gastroprotection in high-risk individuals.5
Although almost all psychotropics can affect the QT interval. Citalopram and escitalopram are particularly associated with interval prolongation in comparison with other SSRIs.11 QT interval prolongation is potentially serious and can be associated with an increased risk of ventricular arrhythmia.
Sertraline, by contrast, is among the safest SSRIs in the context of cardiac disease. Venlafaxine can be a useful medication when an SSRI has proved ineffective. The atypical antidepressant mirtazapine can also be considered as a suitable alternative in the context of failed response to an SSRI,in particular if the aim is to improve sleep and appetite.
In the past the recommendation was to “start low and go slow,” although now evidence suggests that it may not be necessary to titrate upwards so slowly in all individuals. Instead, the goal should be to increase the dose regularly as tolerated at 1- to 2-week intervals in order to reach an average therapeutic dose more quickly.12
If older agents such as TCAs or monoamine oxidase inhibitors (MAOIs) are to be used in the elderly then careful consideration of side-effects (in particular anticholinergic ones, such as delirium), and careful monitoring and supervision may be necessary. This often necessitates referral to secondary care for advice or treatment.
Augmentation of treatment for depression
Lithium is among the most established options for augmentation in treatment-resistant or recurrent depressive disorder, and has a strong evidence base in older adults.13 However, it is associated with a number of adverse effects that the elderly may be more vulnerable to, including lithium toxicity. One should be particularly mindful of the patient’s renal status, and regular blood monitoring as per local guidelines is essential.
While antipsychotics have an established evidence base in augmentation treatment of younger adults with depression, evidence in the elderly is limited.
Managing side-effects of depression medication
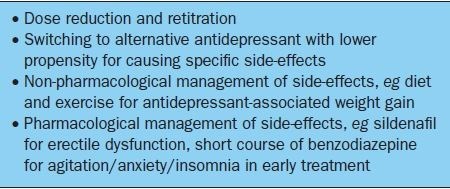
Useful advice for managing persistent, severe or distressing side-effects can be found in the revised British Association for Psychopharmacology (BAP) guidelines for treating depressive disorders with antidepressants14 are summarised in Table 1.
Length of treatment
The evidence base for the optimal length of treatment in older adults is uncertain. NICE guidance recommends continuing antidepressant treatment for at least six months following remission.5 However, NICE also recommends continuing treatment for at least two years in the case of relapse of a recurrent depressive disorder, or if there are risk factors for relapse or the consequences of relapse are likely to be severe.5
Non-pharmacological treatments for depression
Psychosocial interventions are important in the older population. Social isolation and loneliness can be particularly problematic, and referral to social services may be considered to assess for adequate care support at home. Older people’s day-care centres are a vital source of social interaction and activity. NICE guidance recommends that in mild depressive episodes, supportive interventions should be considered first-line, with a stepped approach to offering psychological therapy or antidepressant medication in those that fail to respond.5
In view of the association between elderly depression and chronic physical illness, optimising management of these conditions is important.
Electroconvulsive therapy (ECT) is a safe and effective treatment for depression in the older patient (can be performed as outpatient) that can achieve a good response in 70–90% of cases, though subsequent relapse remains a problem.15 In 2003, NICE recommended the use of ECT for severe depression that has failed to respond to an adequate trial of pharmacotherapy (undefined) or where there is risk to life (through suicide or neglect of diet/fluids).
Most UK old age psychiatrists would attest to it being effective, safe and potentially life saving as short term treatment of severe depression. The mechanism of action is mostly unknown. The neurophysiological changes that occur during ECT found to be similar as those occurring during a successful course of antidepressant medication. Anaesthesia for ECT has a significant effect on its effectiveness.
This option of treatment is often forgotten and being underutilsed even though the side effect rate is much less than with pharmacological treatments. Common side effects include headache, nausea and myalgia. Most patients will have some transient disorientation and some retrograde amnesia. The mortality rate in all patients is said to be 1/50,000. The absolute contraindications to ECT is raised intra-cranial pressure and leaking aneurysm.16
There is some evidence that older people may be less likely to be referred for a talking therapy.5 Although the factors underlying this are not clear, there may be a perception that talking therapies are less effective in older people. It is important to stress that the evidence suggests this assumption is not true. There is strong evidence that psychological therapies are equally effective in old age as in younger adults.17 However, there may be service barriers to accessing therapy, for example for people who are housebound or in care homes.
How long does depression last?
While remission rates in older people are comparable with younger adults, relapse appears to be more common in the older age groups. In a study that followed up subjects for six years, almost half were depressed for more than 60% of the six-year period, with only 23% achieving sustained remission.18
These statistics may seem rather bleak, but there is some evidence that thorough, persistent and sequential treatment for older patients who do not respond to initial treatment can achieve very good rates of remission. One study demonstrated a 84% remission rates in patients who underwent this approach.4
Referral to secondary care
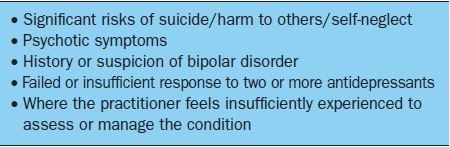
Recommendations on when to refer to secondary care from the BAP guidelines on treating depressive disorders are summarised in Table 2.
In the context of old age, complex psychosocial situations in addition to complexity arising from multimorbidity, frailty and/or cognitive impairment frequently necessitate the expertise of the old age mental health team.
Guidelines/management protocols
Comprehensive guidance on the management of depression can be obtained from the NICE guideline on depression in adults (CG90)5 and the British Association for Psychopharmacology evidence-based guidelines for treating depressive disorders with antidepressants.
Support groups and useful resources
People who are prone to depression often find it helpful to join a local self help group. They can meet up with others who have similar problems and offer mutual support to one another by sharing their feelings, ideas and successes.
The following organisations may hold details of local self help groups in different area:
- Voluntary Services Directory
- Volunteering UK
- Libraries
- GP’s and local clinical commissioning groups
- Mental Health Units/Centres
- Citizens Advice Bureau
- Community and Voluntary Services – (CVS)
- Some national charities also have listings of local mental health groups, such as:
- Mind
- Self Help UK
Conclusion
Depression in old age is a common and disabling disorder that has historically been under-recognised and undertreated. While careful consideration should be given to comorbidities including frailty, treatment is safe and effective and can provide significant benefits in terms of symptoms, quality of life and overall health and wellbeing.
For more news and articles on depression visit our psychiatry section.
Dr Prianka Baral, Trust Grade Registrar in Care of Elderly Department, Watford General Hospital.
References
- https://www.mentalhealth.org.uk/statistics/mental-health-statistics-older-people
- https://www.nia.nih.gov/health/depression-and-older-adults
- The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. World Health Organization, 1992
- Kok R, et al. Outcome of late-life depression after 3 years of sequential treatment. Acta Psychiatr Scand 2009;119(4):274–81.
- National Institute for Health and Care Excellence. Depression in adults: recognition and management. CG90.October 2009 (updated April 2016). Available from: https://www.nice.org.uk/guidance/cg90.
- Hegeman J, et al. Phenomenology of depression in older compared with younger adults: meta-analysis. Br J Psychiatry2012;200(4):275–81.
- https://patient.info/doctor/geriatric-depression-scale-gds
- https://www.stchristophers.org.uk/wp-content/uploads/2015/11/steps_stepfive_geriatric_depression_scale_091.pdf
- Spina E, et al. Clinically relevant pharmacokinetic drug interactions with second-generation antidepressants: an update. Clin Ther 2008;30(7):1206–27
- Mottram PG, et al. Antidepressants for depressed elderly. Cochrane Database Syst Rev2006;1:CD003491.
- Castro VM, et al. QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ2013;346:f288
- https://www.bcmj.org/articles/geriatric-depression-use-antidepressants-elderly
- Cooper C, et al. A systematic review of treatments for refractory depression in older people. Am J Psychiatry2011;168(7):681–8.
- Cleare A, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2008 British Association for Psychopharmacology guidelines. J Psychopharmacol2015;29(5):459–525.
- Flint AJ, Gagnon N. Effective use of electroconvulsive therapy in late-life depression. Can J Psychiatry2002;47(8):734–41
- https://www.gmjournal.co.uk/electroconvulsive-treatment
- Cuijpers P, et al. Is psychotherapy for depression equally effective in younger and older adults? A meta-regression analysis. Int Psychogeriatr2009;21(1):16–24.
- Beekman AT, et al. The natural history of late-life depression: a 6-year prospective study in the community. Arch Gen Psychiatry 2002;59(7):605–11.


