Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
 Introduction
Introduction
What are AFFs?
What causes AFFs?
How common are AFFs?
Management of AFFs
Prevention of AFFs
Conclusion
References
Introduction
Osteoporosis remains a major cause of morbidity and mortality in the UK with approximately 536,000 fragility fractures every year.1 The most commonly prescribed treatment for osteoporosis is bisphosphonate therapy. These medications have been shown to reduce the incidence of vertebral and non-vertebral fractures in the treatment of post-menopausal osteoporosis.2 Bisphosphonates are also used to treat a variety of other metabolic bone diseases including glucocorticoid-induced osteoporosis, Paget’s disease and hypercalcaemia due to a variety of causes, as well as skeletal metastases.3
Over the past decade a number of potential complications have been reported in association with bisphosphonate therapy, including osteonecrosis of the jaw4 and atypical femoral fractures (AFFs).5 There have been more recent links with AFFs and denosumab, a monoclonal antibody used in the treatment of osteoporosis. Osteonecrosis of the jaw is a rarely encountered complication given that it was linked to high dose bisphosphonate therapy for malignancy. Conversely, AFFs are more commonly encountered given their association with low dose bisphosphonate therapy used to treat osteoporosis.
Prevention of AFFs
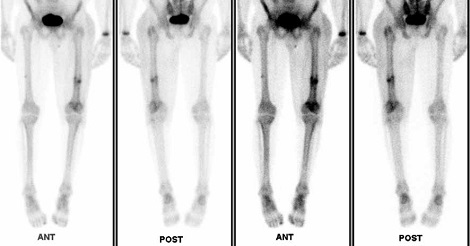
The American Society of Bone and Mineral Research (ASBMR) developed a case definition in 20095 and recently updated this in 2013.6 To satisfy the case definition of AFF, the fracture must be located along the femoral diaphysis from just distal to the lesser trochanter to just proximal of the supracondylar flare. In addition, four out of five major criteria must be fulfilled (Table 1). Four minor criteria are also contained in the case definition, but are not required for diagnosis. AFFs are characterised by unique radiographic and clinical features that make them distinct from osteoporotic femoral fractures. The radiographic features are the transverse orientation, general lack of comminution and localised cortical thickening at the fracture site. (Figure 1) Distinguishing clinical features are the prodromal pain and bilaterality.
What causes AFFs?
The exact cause of atypical fractures remains unclear, although several mechanisms have been proposed. The most widely accepted view point is that AFFs represent a type of stress or insufficiency fracture. Stress fractures imply the idea of abnormal loading on normal bone while insufficiency fractures imply normal loading on abnormal or deficient bone. Exercise-induced femoral stress fractures are normally seen on the medial aspect of the femur. However, AFFs differ in that they always begin laterally and extend medially as they progress from incomplete to complete AFFs.
These fractures begin as microcracks within the bone cortex and the normal healing process involves targeted remodelling through the action of osteocytes. However, bisphosphonates main action on bone is to inhibit osteoclastic activity and therefore suppress bone remodelling. Since bisphosphonates will accumulate at sites of high bone turnover including areas of stress fracture,7 the microcracks are not adequately repaired. Over time these can coalesce and become a more critical cortical defect and thus precipitate a fracture.
| TABLE 1: ASBMR TASK FORCE 2013, REVISED CASE DEFINITION OF AFFS |
|---|
|
Major features
|
Minor features
|
How common are AFFs?
Incidence of these fractures has been difficult to ascertain. One way of doing so is through the use of large registries or databases using ICD-9 codes. This has been found to be inaccurate with specificity for identifying subtrochanteric and femoral shaft fractures quoted as low as 36% in some studies.8 Other studies looking at incidence have used radiographic review to appropriately categorise fractures. These are generally limited due to smaller size and other biases.9 One large dual-centred retrospective study looking at 3,515 cases reported 11.5% of proximal femoral fractures to be in the subtrochanteric or femoral shaft region and of those only 7% identified as AFFs. 81% of those AFF patients were on treatment with bisphosphonates with mean duration of 4.6 years.10
There have been significant associations with AFFs and bisphosphonate use. Relative risk is fairly high in these patients, ranging between 2.1 to 128. This means that there is a high chance of a patient presenting with an AFF having a history of bisphosphonate use. But the absolute risk is extremely low, ranging from 3.2 to 50 cases per 100,000 patient years. AFFs associated with bisphosphonate use are rare when compared with the incidence of common osteoporotic fractures. Clinicians should therefore not be reluctant to prescribe bisphosphonates when indicated, despite the links with AFFs. More importantly there is an increasing association between AFF and bisphosphonate duration. The ASBMR taskforce reported an increase from two per 100,000 cases per year after two years bisphosphonate use, up to seventy-eight per 100,000 cases per year after eight years of use.6
Management of AFFs
Patients who present with complete AFF should be managed with surgical fixation. If the use of antiresorptive agents in the form of prolonged courses of bisphosphonates or denosumab has been identified, these should be stopped immediately. It is crucial that all patients with complete AFF must have bilateral imaging performed due to the high risk of bilaterality. The original task force review of literature in 2010 reported that 28% patients had bilateral fractures and bilateral radiographic abnormalities.5
Management of incomplete AFFs largely depends on pain levels. Prophylactic nail fixation is recommended for all incomplete AFFs accompanied by pain. If the patient has minimal or no pain, a trial of conservative therapy may be considered. In those with minimal pain a period of limited weight-bearing can be undertaken and close follow-up must be organised. If there is no symptomatic or radiographic improvement within 2-3 months, prophylactic nail fixation should be strongly considered due to the risk of progression to complete AFF. In patients with no pain, limited weight bearing may be continued with advice to avoid vigorous activity and this should be continued until there is no bone oedema identified on MRI or increased activity detected on bone scan.
There have been a number of anecdotal reports of AFFs being treated with medical therapy mainly with teriparatide (TPTD). However, in the absence of randomised controlled trials no definite conclusion can be reached regarding this therapy. The ASBMR recommendations for medical therapy are discontinuation of bisphosphonates, adequate calcium and vitamin D supplementation and consideration of TPTD in those who appear not to be healing with conservative therapy.
Fig 1a. Plain radiographs showing complete AFF left femur and incomplete AFF contralateral femur
Prevention of AFFs
Since such a high proportion of AFFs are linked with bisphosphonate use this is the area of greatest importance in the prevention of AFFs. Bisphosphonates should be prescribed in a timelimited fashion for 3-5 years initially (three years for zolendronic acid and five years for other bisphosphonates) with subsequent review thereafter.1 At this stage a drug holiday can be considered with the potential to re-treat with bisphosphonates at a later stage. If fracture risk remains high bisphosphonates can be continued on up to a total of 7-10 years with caution. At this stage it may be of benefit to consider referral to a specialist osteoporosis service for consideration of other agents.
It is crucial that clinicians have a high index of suspicion of AFF in any patients presenting for medical assessment of hip, thigh or leg pain with a history of prolonged bisphosphonate use. These patients should be referred for timely imaging. Patients with incomplete or complete AFF should have bilateral imaging due to the high likelihood of bilaterality. This is useful to ensure incomplete AFF on the contralateral leg is not missed as this could progress to complete AFF in the future.
Conclusion
AFFs are felt to be a type of stress or insufficiency fracture with a high proportion linked to prolonged bisphosphonate use. AFFs can present with prodromal pain and if identified bilateral imaging should be requested. Overall, the treatment of AFFs is largely surgical however bisphosphonates should be discontinued and other osteoporotic agents considered if necessary. Despite the risk of AFF in those using bisphosphonates it must be highlighted that the benefit of bisphosphonates in preventing osteoporotic fractures by far outweighs the risks of AFFs. Bisphosphonates should continue to be used in appropriate patients with the emphasis being on time-limiting the prescription.
Dr Philip Wilson, Orthmedicine Specialty Doctor, Fracture Unit, Royal Victoria Hospital, Grosvenor Road, Belfast
Dr Gary Heyburn, Orthomedicine Consultant, Fracture Unit, Royal Victoria Hospital, Grosvenor Road, Belfast
Conflict of interest: none declared
References
1. National Osteoporosis Guideline Group (NOGG) Clinical Guideline for the prevention and treatment of osteoporosis 2017. Available at: https://www.sheffield.ac.uk/NOGG/downloads.html [Accessed June 2017]
2. Harris ST, Watts NB, Genant HK et al. Effects of risedronate treatment on vertebral and non-vertebral fractures in women with post-menopausal osteoporosis: a randomized control trial. Vertebral Efficacy with Risedronate Therapy (VERT) study group. JAMA 1999; 282(14): 1344–52
3. Unnanuntana A, Saleh A, Mensah K, et al. Atypical Femoral Fractures: what do we know about them. J Bone Joint Surg Am 2013; 95(8):1-13
4. Khosla S, Burr D, Cauley J, et al; American Society for Bone and Mineral Research. Bisphosphonate-associated American Society for Bone and Mineral Research. J Bone Miner Res 2007; 22:1479–91
5. Shane E, Burr D, Ebeling PR, et al. American Society for Bone and Mineral Research. Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2010; 25: 2267–94
6. Shane E, Burr D, Abrahamsen B et al. Atypical Subtrochanteric and Diaphyseal femoral fractures: Second report of a task force of the American Society for Bone and Mineral Research. Journal of Bone and Mineral Research. 2014; 29(1): 1–23
7. Chisin R. The role of various imaging modalities in diagnosing stress fractures. In: Burr DB, Milgrom C, editors. Musculoskeletal fatigue and stress fractures. Boca Raton, FL: CRC Press 2001: 279–94
8. Spangler L, Ott SM, Scholes D. Utility of automated data in identifying femoral shaft and subtrochanteric (diaphyseal) fractures. Osteoporos Int. 2011; 22: 2523–7
9. Abrahamsen B. Atypical femur fractures: refining the clinical picture. J Bone Miner Res. 2012; 27: 975–76
10. Thompson R, Philips J, McCauley S et al. Atypical femoral fractures and bisphosphonate treatment: experience in two large United Kingdom teaching hospitals. J Bone Joint Surgery Br 2012; 94(3): 385–90


