Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Professionals in health and social care are often faced with the challenge of assessing people who have mental health problems along with physical illnesses. These presentations are complex and can be further complicated by issues relating to capacity and consent. The following case brings to light the problems faced by frontline staff when in such circumstances.
While working as a psychiatrist one is frequently asked to assess capacity by medical colleagues for treatment related issues. In most such instances going through the basic principles of the Mental Capacity Act (MCA) is enough. All doctors should be proficient in assessing capacity and managing incapacitated patients.1 However, research suggests that there are gaps in knowledge of this area among doctors across various non-psychiatric specialties.2 For more complex cases psychiatric input can be helpful.
Case history
I was contacted by an out of hour’s GP seeking advice on a 69-year old man in the community, refusing treatment for a gangrenous leg. I advised him to assess his capacity to consent to treatment. They were unsure about the use of MCA hence I explained the basic principles. He felt that using Mental Health Act (MHA) would be more appropriate as the patient was refusing treatment. I explained how this would be inappropriate. There were further calls to clarify if they could “force the patient to go into hospital against their will.”
I was then asked to attend for Mental Health Act assessment as the GP felt he could not assess the patient’s capacity to consent to treatment as he was drowsy. Collateral history was one of excess alcohol use and resulting self neglect.
The man had also been using more than the prescribed dose of morphine due to the severity of the pain. I was concerned enough to discuss the case with the on call Approved Mental Health Professional (AMHP). He was unsure of the appropriateness of the request but under the circumstances agreed to attend. We arrived to find a thin, dishevelled man lying in his own urine.
The house had a fishy odour, from his gangrenous leg. He was drowsy and unable to talk in full sentences. His ability to register any information was compromised. We made the decision to take him to hospital under the MCA. The ambulance staff asked for the “section papers”.
We explained the MCA and inappropriateness of use of the MHA in such circumstances. The ambulance staff were very reflective, identifying that there was little formal training on the MCA. I contacted the Accident and Emergency department to speak to the doctor in charge about his arrival and expressed our concerns. The reply of the doctor was “why are you sending him, if he is not consenting to treatment”. I suggested they consider treating him under The Mental Capacity Act.
Discussion
This scenario has highlighted important issues relating to knowledge, training and the role of the psychiatrist in such circumstances. We came across a range of professionals who have limited understanding on capacity related issues and were hence unable to act in the patient’s best interests. A survey conducted by the Mental Health Act Commission found that general hospitals make use of the Mental Health Act for a relatively small but not insignificant number of patients.3 However, remarkably few studies have addressed levels of knowledge of the Mental Health Act or of capacity and consent in clinicians working in general hospitals.3
The Care Quality Commission has highlighted the importance of training in its guidance notes on this matter and has suggested that this might well be provided in conjunction with a local mental health unit. The Mental Capacity Act 2005 (MCA) was fully implemented in October 2007 in England and Wales. Previous surveys have identified variable levels of training of healthcare professionals on mental capacity and its assessment.2
Emergency healthcare workers do not have adequate knowledge about how to assess capacity and treat people who either refuse treatment or lack capacity.4 There are also concerns about the resulting workload of old age psychiatrists in implementing the MCA and this requires careful monitoring.5
Mental Capacity Act, 2005
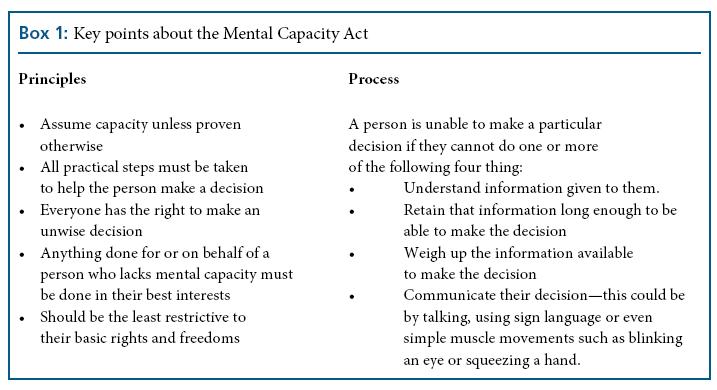
Anyone aged 16 and over may be subject to the Act if they have an abnormality of the mind or brain, which may be affecting their decision-making ability.6 A functional test of mental capacity emphasises the decision and time specificity of capacity. Although the MCA does not identify the decision maker, the Code of Practice assumes the person directly concerned with the decision to be made, to be the decision maker. Hence, everyone who works in health and social care in England and Wales has responsibilities under the MCA. Box 1 summarises key principles and processes for MCA.
Mental Health Act, 1983
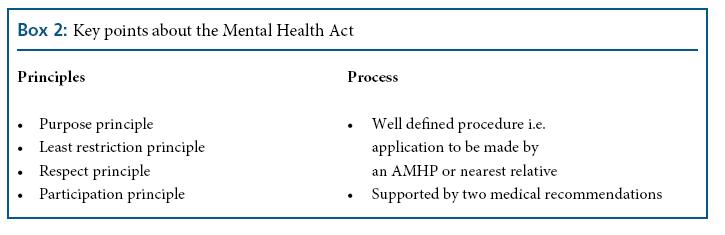
The Mental Health Act is primarily concerned with patients who are diagnosed as having a mental disorder which requires that they be detained or treated in the interests of their own health or safety, or with a view to protecting others. It is also considered when the person lacks capacity to decide on some elements of the treatment but has capacity to refuse a vital part of it.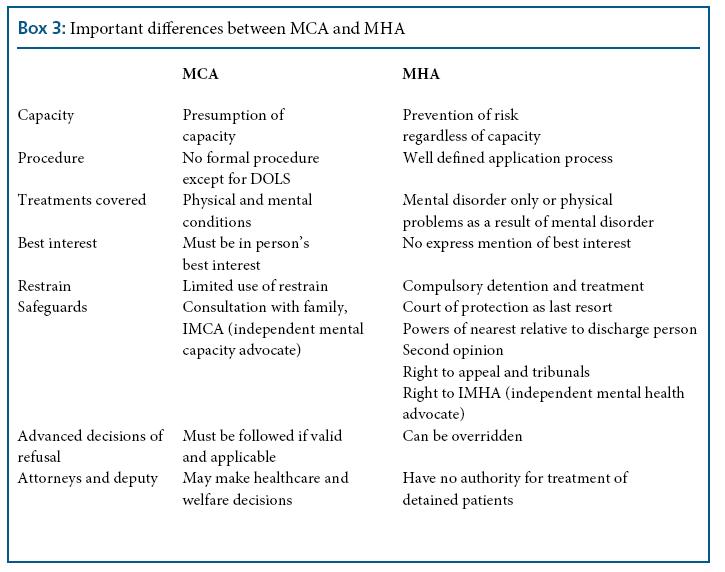
Even people who have capacity to consent cannot refuse treatment for the mental disorder if they are subject to MHA provisions. However any medical treatment can only be offered if the patient consents or is proven not to have capacity, under the MCA. Box 2 summarises key principles and processes in the MHA. Box 3 summarises important differences between MCA and MHA.
Areas of overlap
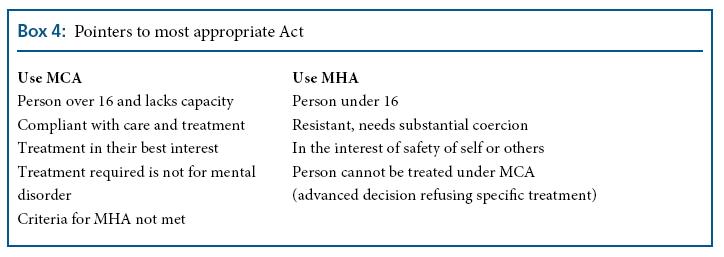
Both Acts may affect people with a mental disorder who need treatment for that disorder, but who lack capacity to make decisions about the proposed treatment. Box 4 summarises useful indicators to the most appropriate legal framework.
Conclusions
The need to assess for mental capacity is a common medicolegal situation requiring skill and training. Moreover, assessing mental capacity is a generic skill; competence in this should be part of training for all healthcare professionals. Decisions regarding capacity for life-saving treatment in people with psychiatric disorders are of a very complex nature and joint working with psychiatrists on these should be encouraged. Training material is readily available in various public domains along with local training opportunities. The five sets for MCA including a core set, a mental health set, a residential accommodation set, a community care and primary care set and an acute hospital set can be downloaded from the Department of Health website.7 Lastly consideration should be given to statutory provision of training in the application of the MCA by all healthcare and social care providers for all their healthcare and social care staff. For staff working in social care resources are available from the SCIE website.8
Conflict of interest: none declared
References
- Richards F, Dale J, The Mental Health Act 1983 and incapacity: what general hospital doctors know. The Psychiatrist 2009; 33: 176–78
- Lynch RM, Simpson M, Higson M, Grout P. Section 136, The Mental Health Act 1983; levels of knowledge among accident and emergency doctors, senior nurses, and police constables. Emerg Med J 2002; 19: 295–300.
- Mental Health Act Commission. Use of the Mental Health Act 1983 in General Hospitals without a Psychiatric Unit. Mental Health Act Commission 2001: 6
- Evans K, Jackson E, Warner J. How much do emergency healthcare workers know about capacity and consent? Emergency Medical Journal 2007: 24; 391
- Shah A. The early experience of Old Age Psychiatrists in the application of the Mental Capacity Act 2005: a pilot study. International Psychogeriatrics, 22(1), 147–57
- Department of Constitutional Affairs. Mental Capacity Act 2005.Code of Practice. TSO (The Stationery Office), 2007; 2
- http://www.dh.gov.uk/en/ Publicationsandstatistics/ Publications/ PublicationsPolicyAndGuidance/ DH_074491 Accessed 12/02/13 8. http://www.scie.org.uk/ publications/mca/resources/basic. asp Accessed 12/02/13
Authors
- Dr Sandhya Gaur
- Dr Ruchit Sood