Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Introduction
A 74-year-old woman presented with a three-week history of non-resolving myoclonic jerks. In this atypical case the observation of non-resolving myoclonic jerks, evidence of demyelination lesions in the brain and spinal cord, along with lumbar puncture findings of oligoclonal bands confirmed the diagnosis of multiple sclerosis.
Case report
A 74-year-old woman presented to the accident and emergency department with a three-week history of confusion and episodes of myoclonic jerking. During this admission she was diagnosed with myoclonic seizures. She was started on levetiracetam. She initially responded well to this treatment and was subsequently discharged home with the plan to titrate medications in response to her symptoms.
Further reading
One month later she was readmitted to the hospital with worsening of myoclonic jerks, despite increase in the dose of levetiracetam, and diplopia. On examination she had myoclonic jerks affecting her lower and upper limbs, with facial muscles spared. She showed no evidence of cognitive impairment, cranio-bulbar weakness, nystagmus, or pyramidal weakness. Her blood tests were unremarkable.
She was commenced on sodium valproate by the neurology team with partial improvement in myoclonic jerks. She underwent electroencephalography (EEG) which showed nonspecific frequent slow transients over the right posterior quadrant and occasional independent bursts of slow waves over the left fronto-temporal areas, suggesting of focal cerebral dysfunction.
Magnetic resonance imaging (MRI) of her brain and cervical spine showed high signal lesions within the deep white matter and cervical spine suspicious of demyelination (figure 1 and figure 2).
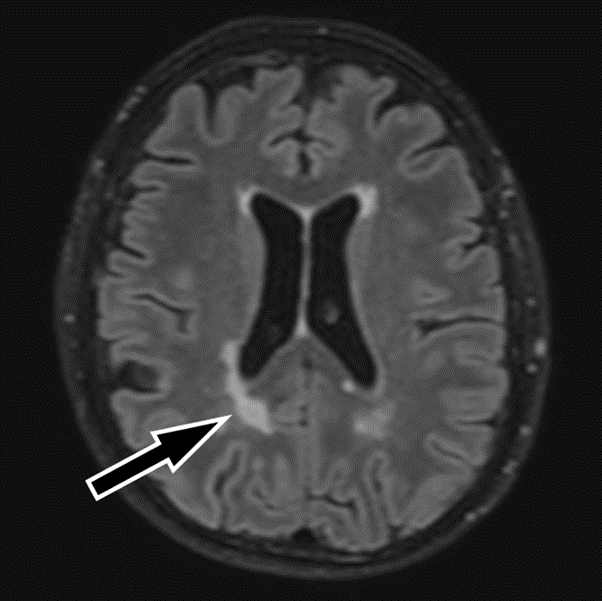
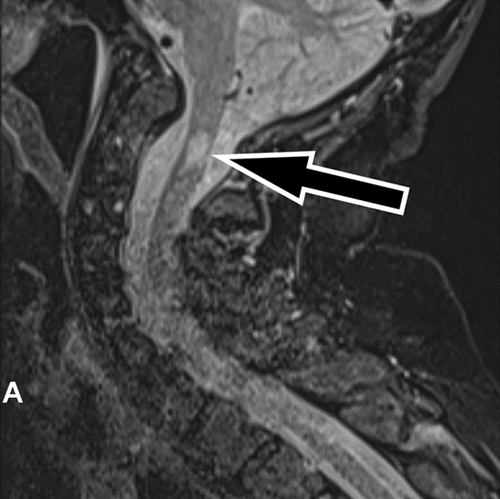
These reports were discussed at a meuroradiology multidisciplinary team meeting. It was felt that the images were suggestive of a demyelinating pathology. A lumbar puncture was carried out. Cerebrospinal fluid analysis was unremarkable with glucose 4.1mmol/L (2.8 – 4.4mmol/L), protein 0.41g/L (0.15-0.45g/L), lactate 1.8mmol/L (1.1-2.4mmol/L), lactate dehydrogenase 25U/L (
A neurology auto-immune screen was undertaken which was also unremarkable (AP4 antibodies negative, Gaba-b antibodies negative, Glycine receptor antibodies negative, Myelin oligodendrocyte antibodies negative, Anti Ampa1 antibodies negative, Anti Ampa2 antibodies negative). She was commenced on IV methylprednisolone with good clinical response. She was discharged home with follow up by the neurology team.
Discussion
Multiple sclerosis usually presents in younger population 20 to 40 years old.1 When the diagnosis of MS is made after the age of 50, it is called late onset multiple sclerosis (LOMS). The prevalence of LOMS is around 4.6%-9.6%.2 The diagnosis of LOMS is usually delayed compared to younger patients leading to delay in treatment and worsen prognosis.3
Myoclonic jerks are a rare presentation of MS. This presentation poses a diagnostic challenge when it presents at the disease onset and has a wide range of other differentials such as epilepsy, autoimmune inflammatory conditions, metabolic disorders, medication induced, renal or liver failure.
However, in this case, an older patient presented with myoclonic jerks and was subsequently diagnosed with LOMS. Evidence for this diagnosis included observation of two separate episodes of non-resolving myoclonic jerking, demyelinating lesions in the brain and spinal cord with location correlating with presenting symptoms, and lumbar puncture findings of oligoclonal bands confirmed the diagnosis of MS based on revised McDonald criteria.4
Learning points
- Myoclonic jerks are rare presentation of multiple sclerosis
- Late onset multiple sclerosis (LOMS) can present with atypical signs and symptoms due to overlaps with mental and physical changes associated with ageing.
- Myoclonic jerks pose a diagnostic challenge when it presents at the disease onset as has a wide range of other differentials such as epilepsy, autoimmune inflammatory conditions, metabolic disorders, medication induced, renal or liver failure
References
- Roohani P, Emiru T, Carpenter A, et al. Late onset multiple sclerosis: Is it really late onset? Multiple Sclerosis and Related Disorders 2014; 3(4): 444–49 https://doi.org/10.1016/J.MSARD.2014.02.004
- Martinelli V, Rodegher M, Moiola L, Comi G. Late onset multiple sclerosis: clinical characteristics, prognostic factors and differential diagnosis. Neurological Sciences : Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology 2004; 25(4) https://doi.org/10.1007/S10072-004-0339-8
- Meca-Lallana V, Berenguer-Ruiz L, Carreres-Polo J, et al. Deciphering Multiple Sclerosis Progression. Frontiers in Neurology 2021; 12. https://doi.org/10.3389/FNEUR.2021.608491/FULL
- Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. The Lancet. Neurology 2018; 17(2): 162–173. https://doi.org/10.1016/S1474-4422(17)30470-2
Emilia Robinson, Department of Health and Ageing, East Sussex Healthcare NHS Trust, St Leonards on Sea
Sanka Vijayabandara, Department of Age and Ageing, East Sussex Healthcare NHS Trust, St Leonards on Sea
Muhammad JH Rahmani, Department of Health and Ageing, East Sussex Healthcare NHS Trust, St Leonards on Sea


