Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
 Introduction
Introduction
DNA Vaccines
Artifcial pancreas
Conclusions
References
Introduction
Around 90,000 people in the UK live with type 1 diabetes. Many sufferers develop the condition in childhood or young adulthood, and the condition can lead to increased risk of micro- and macrovascular complications, with a reduced life expectancy of 11–14 years.1
With support and careful management, however, many people with the condition lead healthy and fulfilling lives. Nevertheless, the need for daily frequent glucose tests and insulin injections can have an adverse impact on quality of life.
More than one in five cases of type 1 diabetes are diagnosed in people aged over 40, according to new figures announced recently at Diabetes UK’s annual Diabetes Professional Conference.
Before insulin was discovered in 1922, the diagnosis of type 1 diabetes led to an inevitable death. Type 1 diabetes occurs when pancreatic beta cells are subject to an autoimmune attack of unknown origin. This leads to pancreatic beta cell failure, and loss of insulin secretion.
By the time symptoms develop, around 90% of beta cells are destroyed. Many hypotheses abound as to the cause of this autoimmunity, and a significant amount of research has been targeted towards preventing or ameliorating the condition.2 We briefly review two recent advances; the potential of DNA vaccines to prevent type 1 diabetes, and the potential of the artificial pancreas to treat established type 1 diabetes.
DNA vaccines
Since the inception of vaccination by Edward Jenner in the 18th century, its role has been to enhance immunity against foreign pathogens. Today, vaccines are being considered for use against long-term, progressive diseases as opposed to the infectious disease killers of Jenner’s day.
We have become accustomed with vaccines being used to help prevent infectious disease, so the notion of them being used to treat type 1 diabetes may be unfamiliar. Researchers are now exploring the potential for vaccination to down regulate autoimmunity. Vaccines work by injecting a live or attenuated antigen from a known pathogen in hope that the body’s immune system would familiarise itself with the pathogen and mount an effective response if it was to ever come in to contact with the real pathogen. The opposite effect may now be achieved in autoimmune diseases such as type 1 diabetes with the advent of DNA vaccines.
DNA vaccines utilise the body’s own immune system to introduce and prime itself towards future infections. A sequence of DNA is inserted via biological vehicle that carries the DNA to cells; this carrier is known as an adjunct.
Once the DNA reaches the target cell it incorporates its genetic material into the genome of the host, in a process similar to viruses and is then decoded by the cells internal machinery to produce proteins representative of the original pathogen.3 This inserted DNA strand is taken from a pathogen against which we need protection, and once it has been translated into a protein it will be presented on the surface of antigen presenting cells for other immune cells such as B and T lymphocytes to identify. Just as we are able to recognise an elephant by its trunk, the immune system will now be able to recognise an invading pathogen by one of its key components.
There are a number of advantages of using a DNA vaccine as opposed to conventional vaccines.4
- Absence of any infective agent
- Effective immune response due to stimulation of both B and T lymphocyte cells
- DNA vaccines are much less sensitive to temperature and other environmental conditions
- DNA can be easily replicated permitting large scale manufacture.
A recently reported ground breaking study examined whether DNA vaccines could be used to dampen the autoimmune response against beta-cells in type 1 diabetes.5 The researchers used a DNA plasmid with a pro-insulin gene, delivered via intramuscular injections in to the beta-cells of the pancreas.
Pro-insulin is the precursor to insulin, and is one of the components targeted by the immune system in type 1 diabetes; by inserting this gene, scientists aimed to increase tolerance towards pro-insulin and therefore reduce the destruction of beta-cells by CD8+ T cells.
The study examined 80 adults over 18 years, who had a diagnosis of type 1 diabetes for longer than five years. Twice as many patients received the DNA vaccine with the active pro-insulin component compared to the control group who received a plasmid injection without the pro-insulin gene.
Patients were given different doses of the vaccine every week for 12 weeks and their progress was monitored by C-peptide levels. Levels of C-peptide increased significantly during the 12 week trial and 3 weeks thereafter by 19.5% in the group given the vaccine compared to an 8.8% reduction in those on the placebo. This suggests that the vaccine not only prevented the deterioration of insulin secretion seen in type 1 diabetes, but actually resulted in an increase in insulin levels. No adverse effects were reported. The vaccine was able to specifically reduce levels of CD8+ pro-insulin T cells whilst maintaining the levels of the other components of the immune system.
Other studies have attempted to modulate the immune response in type 1 diabetes but with little success, such as trials of administering oral insulin to help increase tolerance. The implications of this DNA vaccine are significant but further research is required to establish whether a permanent increase in insulin secretion can be achieved and also whether the rise in insulin/C-peptide levels has a clinically meaningful effect (ie. a reduction in dose of administered insulin or even cessation of insulin injection use).
There is also potential for using such a vaccine in patients at high risk of type 1 diabetes, such as first degree relatives of patients with type 1 diabetes to reduce their risk of developing type 1 diabetes or reduce disease progression.
Artificial pancreas
Endocrine control of glucose is complex, but extremely sensitive, such that normal levels of glucose are maintained in a narrow range in healthy individuals. Pancreatic islets act not only as detectors of glucose levels, but also as a reservoir for hormones that can fine control glucose levels to this narrow range.6
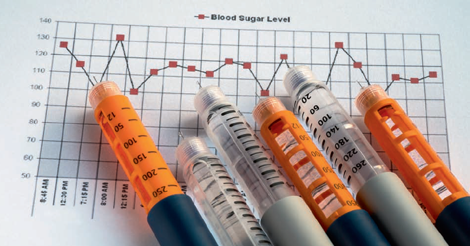
Could we find an artificial way of achieving this—a so-called ‘artificial pancreas’? We currently have widely available technology that can test interstitial glucose levels subcutaneously (a ‘glucose sensor’), which can then send this information wirelessly to a device that delivers insulin continuously under the skin (an ‘insulin pump’). The next challenge is to have a method of making the glucose sensor tell the insulin pump how much insulin to deliver.
This has proven to be a challenge, but progress has recently been made. A control algorithm (a formula which calculates the amount of insulin that needs to be administered according to the blood glucose level) is being tested in clinical trials of patients with type 1 diabetes.7 Results so far have concluded a proof of concept, with safe levels of glucose managed with such a system worn in controlled conditions overnight.8
There are a number of issues that need to be addressed before the system can be used routinely. One issue is that insulin may not be absorbed quickly enough—it can take 90 to 120 minutes for the administered insulin to reach its full potential.
The time lag between the monitor picking up the fact that insulin needs to be delivered and the time when the insulin starts working is often too long. This can lead to high glucose levels when insulin absorption is too slow, or low glucose levels, when the monitor reads high levels, and requests too much insulin.
This time lag may vary from person to person, and hence the algorithm may need to be adapted for each individual. A further concern is infection at the site of insertion of pump or sensor, which may be overcome by covering the sensor with smart materials coated with antibiotics. There are also concerns about how to recharge the battery of the implanted devices.9
Conclusions
Type 1 diabetes is a tough condition. The mantra conveyed to many patients is ‘stay well until there is a cure’. Developing a cure, or making type 1 diabetes easier to manage for the millions of people affected by it worldwide, would have a huge positive impact on people’s lives. Recent advances in DNA vaccines and the artificial pancreas suggest that better management or even a cure is certainly a possibility in the near future.
Mohammed Qurashi,
Aisha Chowdhury,
Tahseen Chowdhury,
Department of Diabetes and Metabolism, The Royal London Hospital, London
Conflict of interest: none declared
References
1. Loacara S et al. Improvements in life expectancy in type 1 diabetes patients in the last six decades. Diabetes Res Clin Pract 2009; 86: 146–51
2. Yoon JW, Jun HS. Autoimmune destruction of pancreatic beta cells. Am J Ther 2005; 12: 580–91
3. Coban C, Koyama S, Takeshita F, et al. Molecular and cellular mechanisms of DNA vaccines. Hum Vaccin 2008; 4: 453–56
4. Robertson J, Ackland J, Holm A, Guidelines for assuring the quality and nonclinical safety evaluation of DNA vaccines. WHO Technical Report Series No 941. 2007: 57–59
5. Bart O, Roep et al. Plasmid-Encoded Proinsulin Preserves C-Peptide While Specifically Reducing Proinsulin-Specific CD8+ T Cells in Type 1 Diabetes. Sci Transl Med 2013; 5: 191ra82
6. Keller J, Layer P. Human pancreatic exocrine response to nutrients in health and disease. Gut 2005; 54 Suppl 6: 1–28
7. Luijf YM, et al. Day and night closed-loop control in adults with type 1 diabetes: a comparison of two closed-loop algorithms driving continuous subcutaneous insulin infusion versus patient self-management. Diabetes Care 2013; 36: 3882–87
8. Hovorka R, et al, Overnight closed loop insulin delivery (artificial pancreas) in adults with type 1 diabetes: crossover randomised controlled studies. BMJ 2011; 342: d1855
9. Kumareswaran K, et al. Closed-loop insulin delivery: towards improved diabetes care. Discov Med 2012; 13: 159–70


