Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Our skin is a complex structure of cells and proteins that constantly act to protect and maintain the body’s normal function. With ageing skin, there is a gradual decline in the skin’s ability to adequately sustain these processes. The epidermis thins and the amount of collagen previously abundant within the dermis steadily falls. Characteristic wrinkles develop and the skin becomes increasingly fragile. Langerhans cell numbers within the basal layer of epidermis drop, increasing the propensity towards cutaneous infection. It is therefore unsurprising that the prevalence of different skin disorders varies with age.
Diagnosing a rash
The time-course of a rash can give a useful guide to the likely differential diagnosis. Infectious disease and drug reactions are likely to give a short history whereas psoriasis and eczema are likely to have been present for longer (Box 1).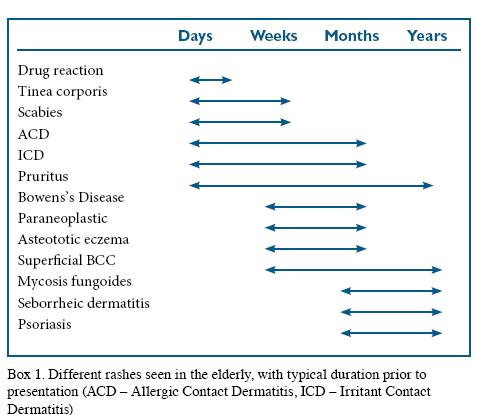
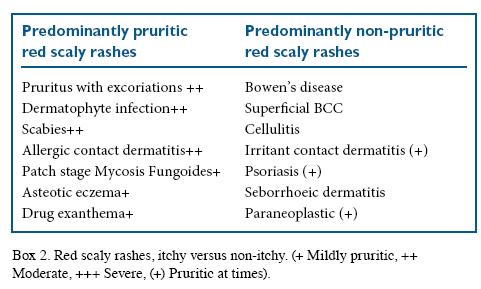
An additional distinction that provides useful diagnostic information is the presence and quality of itch (Box 2). Premalignant or malignant conditions such as Bowen’s disease will usually be asymptomatic. Psoriasis may often be associated with slight itch, but will rarely cause sleep loss due to scratching. Yet sleep loss due to itch is characteristic of eczema.
 Generalised itch (pruritus) is a common complaint among the elderly. The commonest cause of generalised pruritus is xerosis (dry skin), which is easily treated by avoidance of soap products and increased use of emollients. It is critical to distinguish cases of widespread itch with primary skin disease (usually inflammatory) from those with secondary skin disease caused by trauma from chronic scratching (Box 3). Treatment of pruritus relies on the identification of the underlying cause, although this may not always be possible (eg. senile pruritus).
Generalised itch (pruritus) is a common complaint among the elderly. The commonest cause of generalised pruritus is xerosis (dry skin), which is easily treated by avoidance of soap products and increased use of emollients. It is critical to distinguish cases of widespread itch with primary skin disease (usually inflammatory) from those with secondary skin disease caused by trauma from chronic scratching (Box 3). Treatment of pruritus relies on the identification of the underlying cause, although this may not always be possible (eg. senile pruritus).

Aqueous cream with 1% menthol is useful in relieving itch in most cases whereas treatments such as phototherapy may be appropriate in specific cases. In generalised pruritus with excoriations, sparing of the central back is typical because the patient is unable reach this area to scratch without the use of an implement (Figure 1). In chronic scratching, characteristic eroded nodules may develop (nodular prurigo), which are commonly seen on the legs and arms. It is typical for there to be a predominance on the non dominant side. Localised itch may also occur as a consequence of chronic scratching, resulting in a focal area of lichenification and hyperkeratosis (lichen simplex). 
Important pruritic dermatoses in the elderly
Scabies
Scabies is an intensely itchy infestation by human-specific mites. Spread is predominantly through skin-to-skin contact, although mites can survive on clothing and linen for several days. Rapid spread within hospitals and other institutions is common, particularly among the elderly and other immunocompromised individuals. Itching is caused by allergic sensitisation to the mites, excrement or eggs which characteristically takes 2–6 weeks following infestation. Subsequent infestations give rise to a quicker onset of the rash and its symptoms. Erythematous papules and excoriations are characteristic. The characteristic scabies mite burrow is a linear grey thread-like lesion, often with a vesicle at one end, and represents the path of the female mite.
Cutaneous lesions are distributed symmetrically and typically affect the inter-digital web spaces, the flexural aspect of the wrists, the axillae and waist. Nodules on the scrotum and penis, or around areolae are almost pathognomonic. The face is typically spared. Elderly patients who may be immunocompromised or immobile are susceptible to infestation by very high numbers of mites, which may cause thick scaly plaques. This form of scabies is commonly known as Norwegian or crusted scabies and is highly infectious. Surprisingly, the associated itch is often less intense. The atypical presentation can often lead to a delay in diagnosis.
Once the diagnosis of scabies has been made the patient and all household contacts should be treated with permethrin 5% lotion or cream on the same day. This should be applied to the whole body including the head and neck in the elderly and the immunosuppressed. Particular care should be taken to ensure application under the nails and between the fingers and toes. Once applied, it should be left on for between 8 to 12 hours before washing off. Bedding, towelling and clothes should be washed above 50oC. The process is subsequently repeated a week later. In cases of allergy or resistance to permethrin, malathion 0.5% aqueous liquid can be used. Following eradication, crotamiton or topical corticosteroids can be used to control the itch, which may persist for several weeks after successful treatment.1
Psoriasis
The onset of psoriasis shows a bimodal pattern. Late onset psoriasis (peak at 55 years) may often not show the characteristic well demarcated, scaly erythematous plaques over the extensors, scalp, postauricular sites and umbilicus (Figure 2). Late-onset psoriasis also shows a weaker genetic predisposition. Specific clinical findings such as nail changes and koebnerisation are useful positive findings. Solitary plaques of psoriasis need to be distinguished from Bowen’s disease, superficial basal cell carcinoma and dermatophyte infections.

Seborrhoeic dermatitis
Seborrhoeic dermatitis is a common condition typically confined to sites of increased sebum production. The pathogenesis of this disorder remains unclear, but an association with increased numbers of malassezia (pityrosporum) yeasts is recognised. Seborrhoeic dermatitis associated with Parkinson’s disease, mood disorders and HIV is often more treatment resistant.2 The scalp is the most frequently affected site and presents with a fine white scale and a diffuse mild erythema.
Facial involvement is often striking by its symmetry, with an ill-defied greasy scale of the forehead, inner eyebrows, nasolabial folds and ears, external auditory canal and post-auricular areas. When present on the chest and intertriginous areas (axillae, groin and inframammary sites), lesions have an orange-brown colour and may resemble flexural psoriasis. More rarely a generalised form of the condition may occur, giving rise to erythroderma. Treatment is directed at reducing the inflammation and tackling the overgrowth of yeast. Low strength topical steroids, such as hydrocortisone 1% cream, in combination with an imidazole to the facial lesions and intertriginous zones is beneficial. Twice weekly use of ketoconazole shampoo to the scalp, as well as to the face and trunk help to maintain remission. Second-line therapies include moderate potency corticosteroids, calcineurin inhibitors (tacrolimus or pimecrolimus) and systemic imidazoles.
Asteatotic eczema
Untreated dry skin may progress to asteatotic eczema, which is frequently localised to the lower legs and characterised by a network of shallow cracks in the skin resembling crazy paving (eczema craquelé). In more extensive cases, extension with patchy involvement of the thighs and trunk occurs. The degree of pruritus is variable between patients. Late onset eczema in the elderly is often not associated with atopy. It is important to consider possible underlying causes such as pre-bullous pemphigoid, drug hypersensitivity and paraneoplastic disease in these cases. The avoidance of soaps and irritants, regular emollient therapy and topical corticosteroids are the mainstay of management. Severe cases may need systemic treatment with oral prednisolone or steroid-sparing immunosuppressants.
Mycosis fungoides
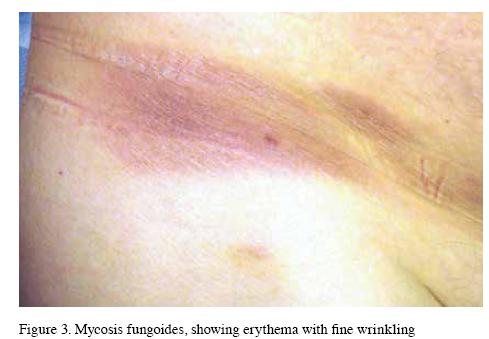
Mycosis fungoides is the commonest form of Cutaneous T-cell Lymphoma (CTCL), with a median age of onset of 55 years. Typically clonal T-cell populations are restricted to the skin thereby representing a “benign” skin limited lymphoma. The disease is usually mildly itchy and progresses from erythematous, fine scaled patches, typically on non-exposed sites to plaques and tumours of the skin. Lesions vary in size and may be difficult to distinguish from tinea corporis, eczema or psoriasis. A fine wrinkled appearance to the surface of affected skin is an important diagnostic clue (Figure 3). In severe cases clonal T-cell populations can be detected in the blood or bone marrow and the prognosis is worse.3
Drug rash
Drug hypersensitivity induced rashes are the commonest cause of new onset rashes in inpatients. Drugs commonly associated with hypersensitivity reactions include Beta-lactam antibiotics, anti-convulsants, allopurinol and sulphonamides. The typical presentation is of a mildly pruritic maculopapular rash starting one to three weeks after the initiation of a new drug. Initially the rash appears on the upper torso and spreads acrally, often becoming confluent. In a limited number of cases it may progress to complete erythroderma. The presence of fever, tender skin, blistering, mucosal involvement or systemic upset are important markers of severity.
Early discontinuation of the causative drug is essential to prevent progression to a more severe drug reaction such as Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS), Stevens-Johnson syndrome or Toxic Epidermal Necrolysis. Rarely, hypersensitivity rashes may develop several weeks after the discontinuation of a drug. Cross reactivity between drugs of the same group or similar structure can induce drug rashes within days of exposure despite never having encountered the drug before.4
Contact dermatitis
Contact dermatitis may be divided into either irritant contact dermatitis (ICD; skin barrier dysfunction) or allergic contact dermatitis (ACD; type IV T-cell mediated hypersensitivity). Both forms potentially pose a problem in the elderly population but ICD accounts for the majority of cases in this age group as it does in the younger population. ICD most commonly affects the hands due to hand washing. In the hospital setting, irritant dermatitis can be induced by the application of antiseptics (chlorhexidine) and low humidity.
In elderly individuals with reduced mobility, faecal and urinary incontinence may give rise to severe dermatitis of the groin, genitals or buttocks. Unlike ICD, ACD is more itchy. Erythema and scaling are typical, with occasional vesiculation. Elderly patients with chronic leg ulcers are at high risk of sensitisation to topical medicaments or bandages and frequently present with lower limb erythema.
Patch testing should be considered in dermatitis with a well defined border, or if affecting the face, hands or genitals because clinical evaluation is often unreliable. Avoidance of the irritant/ allergen and regular application of greasy emollient (such as 30% yellow soft paraffin/30% emulsifying wax) is often adequate. For severe cases topical corticosteroid ointments can be useful.6
Other important rashes
The development of a paraneoplastic rash maybe the first indication that an individual has an underlying neoplasm.
Localised rashes
Tinea corporis and tinea cruris
Dermatophyte (fungal) infections of the skin and nails are common in adults of all ages. Skin lesions are characterised by an itchy, erythematous and scaly lesion (“ring-worm”) except in cases inappropriately treated with topical steroids (tinea incognito). Lesions will typically expand with central clearing and a well defined leading edge, giving rise to an annular or arcuate appearance. Depending on the extent of inflammation, pustules may be also present at the edge of the lesion. The site should be scraped gently with a blade and the scale sent for microscopy and mycological culture. Limited infection can be treated topically with creams such as clotrimazole or terbinafine.
Superficial basal cell carcinoma and Bowen’s disease
Superficial basal cell carcinoma (BCC) and Bowen’s disease (squamous cell carcinoma in-situ; Figure 4) are both localised

well defined discoid areas of scaly skin, usually 1–3cm in diameter. Differential diagnosis includes tinea corporis, eczema or psoriasis. Superficial BCCs show a predilection for the trunk whereas Bowen’s disease is usually on sun exposed sites such as the face, forearms and shins. BCCs usually show a raised edge which is best seen on stretching the skin. In trickier cases a biopsy is helpful in establishing the diagnosis. Management with topical chemotherapies such as 5-fluoruracil or topical imiquimod are often successful. Surgery or photodynamic therapy are also used.
Conclusion
Skin disease in the elderly accounts for a significant proportion of presentations to medical practitioners. This article aims to give the reader a firm basis with which to manage dermatoses in this age group. Thorough examination of patients presenting with red scaly rashes is essential in order to successfully diagnose and alleviate the patient’s symptoms, as well as to ensure that those features indicative of serious underlying pathology are not missed.
Adam Fityan, Michael R Ardern–Jones, Dermatology, University Hospital Southampton
References
- NHS Clinical Knowledge Summaries – Scabies Management. http://www.cks.nhs.uk/scabies/ management/detailed_answers/ managing_scabies/choice_of_ insecticide#-262664
- Malassezia, dandruff and seborrhoeic dermatitis: an overview. RJ Hay. British Journal of Dermatology 2011: 165 (suppl. 2): 2-8
- Joint British Association of Dermatologists and U.K. Cutaneous Lymphoma Group guidelines for the management of primary cutaneous T-cell lymphomas. SJ Whittaker. British Journal of Dermatology 2003; 149: 1095–1107
- Skin manifestations of drug allergy. M Ardern-Jones. Br J Clin Pharmacol 2011: 71(5): 672–83
- Acral violaceous erythema and hyperkeratosis. A Fityan. Clin Exp Dermatol 2011; 36(3): 320–21
- Guidelines for the management of contact dermatitis: an update. J. Bourke. British Journal of Dermatology 2009; 160: 946–54
Conflict of interest: none declared


