Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
Patients with COPD are among the worst affected by COVID-19 and the Global Initiative for Chronic Obstructive Lung Disease (GOLD) is working with the World Health Organization to try to minimise the impact of the infection.
There is no scientific evidence to support that inhaled (or oral) corticosteroids should be avoided in patients with COPD during the COVID-19 epidemic and patients should maintain their regular therapy.
In this blog post, Dr Vincent McGovern, highlights current management of COPD, how to reduce risk factors and impact of comorbidities.
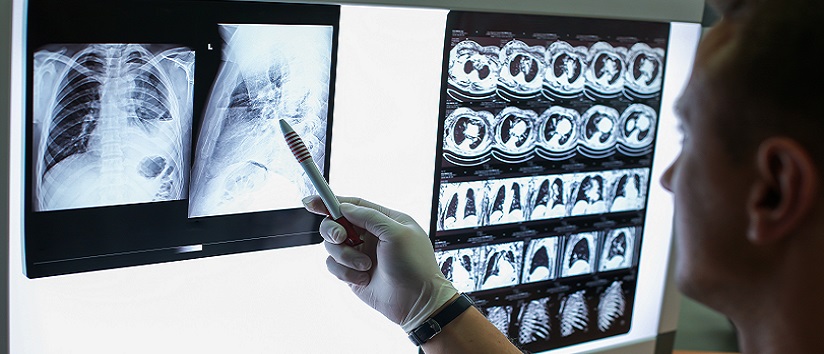
Chronic obstructive pulmonary disease (COPD) is defined by GOLD as: “a common, preventable and treatable disease that is characterised by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.”1
It says that COPD should be considered in any patient who has dyspnoea, chronic cough or sputum production, and/or a history of exposure to risk factors for the disease.1
An estimated 1.2 million people are living with diagnosed COPD in the UK meaning an overall prevalence of 2%.2 This prevalence is increasing year on year, yet studies from the UK and Europe suggest that at least half those affected by COPD are undiagnosed.
Early intervention could preserve lung function and improve other COPD outcomes but diagnosis of COPD in the early stages is limited and it is often only diagnosed when severity has increased. Few GPs perform screening with spirometry with at-risk populations (such as smokers over 40 years) due to inadequate training and resources.3
Smoking cessation has a greater effect when it is achieved earlier in life and further studies are needed to investigate the effects of early treatment in COPD. Advantages of early detection of people with airflow obstruction would be three fold: additional life years saved, greater incentive to quit smoking and quality of life gained.4
Reducing risk factors for COPD
In the initial assessment of a patient, healthcare professionals should exclude alternative causes of symptoms, look for a history of exacerbations and the presence of comorbidities. They should also assess the impact on patient’s life €“ activity, anxiety and mood €“ and whether there is potential to reduce risk factors especially smoking cessation.
The management strategy for stable COPD should be predominantly based on the individualised assessment of symptoms and future risk of exacerbations. All individuals who smoke should be strongly encouraged and supported to quit and the main treatment goals are reduction of symptoms and future risk of exacerbations.1
Management strategies are not limited to pharmacological treatments, and should be complemented by appropriate non-pharmacological interventions.
Bronchodilators are central to the treatment of COPD.5,6 These drugs improve symptoms and quality of life by improving airflow and therefore gas exchange, and by reversing air trapping and dynamic lung hyperinflation.7 There are two classes of long-acting bronchodilators: long acting beta agonists (LABAs) and long acting muscarinic antagonists (LAMAs).
NICE guidance says to offer LAMA+LABA to people who have spirometrically confirmed COPD and do not have asthmatic features/features suggesting steroid responsiveness and remain breathless or have exacerbations despite having used or been offered treatment for tobacco dependence if they smoke. This is in addition to optimised non-pharmacological management and relevant vaccinations and using a short-acting bronchodilator.
An exacerbation of COPD is defined as an acute worsening of respiratory symptoms that results in additional therapy and according to GOLD, these can be precipitated by several factors. The most common causes are respiratory tract infections.
The goal for treatment of COPD exacerbations, therefore, is to minimise the negative impact of the current exacerbation and to prevent subsequent events. Short-acting inhaled beta2 -agonists, with or without short-acting anticholinergics, are recommended as the initial bronchodilators to treat an acute exacerbation.
Maintenance therapy with long-acting bronchodilators should be initiated as soon as possible. Systemic corticosteroids can also improve lung function, oxygenation and shorten recovery time and hospitalisation duration. Duration of therapy should not be more than 5€“7 days. Antibiotics, when indicated, can also shorten recovery time, reduce the risk of early relapse, treatment failure, and hospitalisation duration and should be used for 5€“7€¯days. Following an exacerbation, appropriate measures for exacerbation prevention should be initiated.
Comorbidities and COPD
Reasons for referral from primary care are usually because of diagnostic uncertainty, but other causes include suspected severe COPD, onset of cor pulmonale, dysfunctional breathing, symptoms disproportionate to lung function deficit and frequent infections.
GPs should remember that breathlessness has many causes. Smoking cessation, education, vaccination, inhaler technique and exercise/rehabilitation should all form part of overall management.
Bronchodilation is now the cornerstone of pharmacological treatment to relieve symptoms and inhaled steroids are proven to reduce exacerbations. For some patients, triple therapy in a single inhaler is now available.
We also shouldn’t forget the comorbidities. Anxiety and depression can affect 30-80% patients and are often undertreated. Other comorbidities include cardiovascular disease, lung cancer, diabetes, osteoporosis and muscle wasting and cachexia.
Dr Vincent McGovern, GPwSI, Belfast Trust
Blog based on a talk given at the GM Conference
- GOLD 2019. Global strategy for diagnosis, management, and prevention of COPD
- British Lung Foundation. https://statistics.blf.org.uk/copd
- Calverley PM. Supplementary oxygen therapy in COPD: is it really useful? 2000 Jul;55(7):537-8.
- https://www.nice.org.uk/guidance/NG115
- Singh D. Br J Clin Pharmacol 2015;79:695€“708
- Spina D. Eur Clin Respir J 2015;2:26634
- Disse B et al. Life Sci 1993:52:537€“544



Comments are closed.