Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
 Introduction
Introduction
Criteria for screening a disease condition
Screening for persistent atrial fibrillation
Screening for paroxysmal AF
How much AF is relevant for stroke risk?
Cardiac monitoring for PAF in high risk groups for primary prevention of stroke
Conclusion
Key points
References
This is part 2 of a two-part article.
Part 1 can be found here.
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia affecting about 2.4% of the UK population, with approximately half being undiagnosed. Public Health England (2015) estimates indicate an average GP surgery case burden of 174 (61 undiagnosed). There is a striking increase in prevalence with age, from 10% in the over 75s (see Figure 1).1
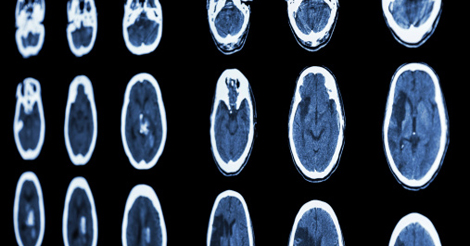
AF is a major risk factor for stroke, increasing the risk five-fold, and about one in five strokes is attributable to AF, increasing to one in two in older age groups. AF-related strokes are more severe, reflected on brain imaging as large cortical infarcts, with a high risk of death (one in four) and residual disability in the majority of survivors. Other complications include: non-stroke systemic embolism, cardiac failure, increased hospitalisation, reduced quality of life, and cognitive decline leading on to vascular dementia.
AF-related stroke satisfies standard criteria for screening,1 as summarised in Table 1. Given the significant societal implications, there needs to be a very good reason for us to “not undertake” screening programs for AF. The importance of prevention of AF-related stroke cannot be over-emphasised.2
Criteria for screening a disease condition
Jung et al set out objective criteria for considering the benefit of screening.2 Prevention of AF is already undertaken in various settings, and is one of the objectives of treating vascular risk factors like hypertension, diabetes and coronary artery disease. It is also one of the goals of lifestyle modification changes like smoking cessation, alcohol moderation and weight loss (in the context of obesity). Optimal targets should be targeted, including: blood pressure 75 years) and HbA1c
Screening for persistent atrial fibrillation
The initial focus should be on identifying persistent AF, which is easily detectable by a pulse examination and can be confirmed by an electrocardiogram (ECG), a universally available and inexpensive test. The majority of embolic complications (chiefly embolic stroke) are eminently preventable with a single intervention: anticoagulation (25 strokes prevented per 1000 people with no prior stroke or TIA; and 90 vascular events prevented, mostly strokes in those with a history of prior stroke or TIA, every year).3,4 This benefit far outweighs the increase in bleeding rates secondary to anticoagulation. In addition, many of the significant practical limitations of the traditional single option of warfarin have now been addressed by four new agents (direct oral anticoagulants: DOAC), all of which are approved by NICE.5 Thus, the only persistent contraindication to anticoagulation is an irremediable structural cause of bleeding. Other contraindications like active bleeding, recent bleeding, and history of remote bleeding are no longer considered absolute; and should be subject to a full review in light of details from prior medical history. In some cases, a structural cause for bleeding may need to be excluded (eg. upper GI endoscopy to confirm healing of previous ulcers).
| TABLE 1. STUDIES INVESTIGATING SCREENING FOR PERSISTENT AF | |||||
|---|---|---|---|---|---|
| Study | Subjects | Strategy | Prevalence | AF detection rate | Comments |
| SAFE Study6,12 | Over 65s in primary care UK | Systematic ECG for all; opportunistic (pulse check, ECG if irregular) | 7.2% | Systematic screening 1.62% Opportunistic 1.64% Control 1.02% |
|
| SEARCH AF13 | Age > 65 years Australia |
Pharmacist pulse palpation and iPhone single-lead ECG | 6.7% | New AF 1.5% | New AF CHADSVASC ≥ 2: 100% Started A/C: 60% |
| STROKESTOP14 | Age 75-76 Sweden |
Mass population screening Handheld ECG for 2 weeks, twice recordings + symptom guided |
9.3% | 3% new AF 2% untreated known AF |
Started A/C: 93% new AF 47% known AF |
Whilst there are several guidelines elucidating the appropriate assessment and management of AF, there is virtually no formal guidance on AF screening. On the whole, there is uncertainty about the cost effectiveness of routine screening, and approaches targeted at high risk groups are likely to result in higher case-detection rates and consequently lower cost per case detected. There is no uniform agreement on the definition of “high risk” for screening programmes. A summary of AF detection rates in recent studies is presented in Table 1. Opportunistic pulse checks in older age groups alongside other interventions (eg. annual flu jab) have been demonstrated to be as effective as, but cheaper, than routine pulse checks6 and are recommended by European Guidelines.7,8 Whilst pulse checks may have significant time implications in primary care, especially if considering routine screening for all, novel devices can enable AF screening within the context of standard practice eg. automated AF detection algorithms incorporated into automated BP measurement devices, like WATCH BP Home.9 It is estimated that routine use of the WATCH BP device could prevent 221 strokes per year, equating to a net saving of £11.6 million annually. In addition, the advent of apps that can identify AF using single lead ECG (AliveCor10), or even beat-to-beat variation in facial skin colour (Cardiio Rhythm11) open up the possibility of self- screening for AF.
Screening for paroxysmal AF
Episodic or paroxysmal AF (PAF) may require repeated assessments and long-term cardiac monitoring, which can be costly. Cardiac monitoring is undertaken when there is a clinical suspicion of PAF based on the clinical presentation eg. episodic palpitations, dyspnoea or chest pain; syncope or pre- syncope, recurrent unexplained falls etc. In addition, there is growing evidence to support prolonged monitoring in the setting of cryptogenic stroke. Prolonged monitoring after cryptogenic stroke or TIA identifies a significant number of people with atrial fibrillation, as summarised in Table 2. Detection rates increase with duration of monitoring undertaken (see Table 3), though robust cost-effectiveness analysis to support the duration of optimal monitoring are not available at present.
| TABLE 2. MAJOR STUDIES OF CARDIAC MONITORING FOR PAF DETECTION FOLLOWING CRYPTOGENIC STROKE | ||||
|---|---|---|---|---|
| Study | Subjects | Strategy (comparator) | AF detection | Comments |
| Gaillard et al15 | Cryptogenic stroke (MRI+) | Transtelephonic EKG (random recordings; 1 per month) | >32s AF: 9.2% | A/C started: 100% |
| EMBRACE16 | Cryptogenic stroke or TIA ( | ELR (24h Holter) | >30s AF: 16.1% (3.2%) >2.5min AF: 9.9% (2.5%) |
Doubling of A/C usage |
| CRYSTAL AF17 | Age > 40 Cryptogenic stroke | ICM (24h Holter) | 6m: 8.9% (1.4%) 12m: 12.4% (2.0%) |
– |
| ELR external loop recorder; ICM insertable cardiac monitor; m months; min minutes; s seconds | ||||
How much AF is relevant for stroke risk?
| TABLE 3. RATE OF DETECTION OF AF FOR VARIOUS PERIODS OF MONITORING18 | |
|---|---|
| Duration of monitoring | AF detection rate |
| Daily ECG x6 | 0.06% |
| 24h monitoring | 3.6% |
| 24h monitoring x6 | 2% |
| 7 day Holter x2 | 4% |
| 72h monitoring | 6.7% |
| 7d monitoring | 7.4% |
| 30 day | 14.3% |
| Implanted device 1 year | 18.3% |
There remains uncertainty about the prognostic value of brief periods of AF, and the question about how much duration of AF constitutes significant stroke risk has not yet been answered. Since prior stroke is the most potent risk factor for future stroke, clinical decisions tend be based on a history of prior stroke. In the setting of previous stroke, patients with brief periods of AF (>30 seconds) have intermediate stroke risk (between non-AF and persistent AF),19 and are generally deemed by stroke physicians to be adequate to recommend anticoagulation.20 For primary prevention, longer durations (>5-6 minutes) are felt to be relevant from observational studies as summarised in Table 4.
Cardiac monitoring for PAF in high risk groups for primary prevention of stroke
No study has explored the potential value of prolonged cardiac monitoring in the general population. It is unlikely that routine prolonged cardiac monitoring in the absence of a prior cryptogenic stroke or TIA will be cost effective.
| TABLE 4. RECENT STUDIES OF CARDIAC MONITORING FOR PAF DETECTION FOR PRIMARY PREVENTION OF STROKE | |||||
|---|---|---|---|---|---|
| Study | Patient group | Study duration | AF rate | AF Duration | HR (outcome) |
| ASSERT21 | Age ≥ 65years; hypertensives | 3 months | 10.1% | > 6 minutes | 2.5 (Ischaemic stroke or systemic embolism) |
| MOST22 | Sinus node dysfunction | 27 months | 51.3% | > 5 minutes | 2.8 (death or nonfatal stroke) |
| TRENDS23 | Indication for implantable cardiac monitor; CHADS2 ≥ 1 | 17 months | 43% | > 5.5 hours | 2.2 (thromboembolism) |
Conclusion
AF portends a grave prognosis, substantially increasing stroke risk. In the presence of a potent intervention to reduce risk, a programme for screening is required. Population-based screening is not considered cost effective, thus targeted screening for AF is recommended as part of a comprehensive approach to stroke prevention in people with AF. It is crucial that identification of AF leads on to appropriate risk assessments to inform anticoagulation decisions. For persistent AF, pulse checks should be targeted at high risk groups perhaps in the context of other assessments (opportunistic). For paroxysmal AF, a structured approach to prolonged cardiac monitoring is required in the setting of previous stroke to reduce risk of recurrent stroke. The value of prolonged monitoring as screening in the general population is currently unclear.
Key points
- There is significant potential for health benefits from screening for AF, however, systematic screening of the whole population is unlikely to be feasible or cost-effective, both for persistent and paroxysmal AF.
- Targeted screening is recommended, focused on populations where presence of AF would identify significant risk of stroke and indicate anticoagulation. For persistent AF, target groups (all over 75s; and all with age 65-75 AND a risk factor, as incorporated in the CHADSVASC Score) should have a pulse rhythm check as part of annual health checks. For paroxysmal AF, target groups (history of cryptogenic stroke/TIA or symptoms suggestive of paroxysmal AF) should lead to prolonged cardiac monitoring, the duration of which remains unclear especially with respect to cost-efficacy.
- The excuse of poor management of known AF is no longer a reason to “not screen”, but indicates the need to improve our response to identified AF. The availability of newer anticoagulants makes anticoagulation therapy more acceptable to users and clinicians alike, as they surmount most of the practical obstacles to warfarin therapy and monitoring.
James J, Fotherby M, Mistri AK
University Hospitals of Leicester NHS Trust
Conflict of interest: none declared
References
1. Wilke T, et al. Incidence and prevalence of atrial fibrillation. Europace 2013; 15: 486–93
2. Wilson JMG, Jung G. Principles and Practice of Screening for Disease, World Health Organization, 1968
3. Aguilar MI,Hart R. Oral anticoagulants for preventing stroke in patients with non-valvular atrial fibrillation and no previous history of stroke or transient ischemic attacks. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No.: CD001927. DOI: 10.1002/14651858.CD001927.pub2
4. Aguilar MI, Hart R. Oral anticoagulants for preventing stroke in patients with non-valvular atrial fibrillation and no previous history of stroke or transient ischemic attacks. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No.: CD001927. DOI: 10.1002/14651858.CD001927.pub2
5. Atrial fibrillation: management. NICE CG180 – nice.org.uk/ guidance/cg180 (accessed 12th May 2017) 6. Fitzmaurice DA, et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ 2007; 335(7616): 383
6. Fitzmaurice DA, et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. BMJ 2007; 335(7616): 383
7. Camm AJ, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: An update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J 2012; 33 (21): 2719–47
8. Kirchhof P, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016; 37 (38): 2893-2962. https://doi.org/10.1093/eurheartj/ehw210 (accessed 12th May 2017)
9. Stergiou GS, et al. A tool for reliable self-home blood pressure monitoring designed according to the European Society of Hypertension recommendations: The Microlife WatchBP Home monitor. Blood Pressure Monitoring 2007; 12(2): 127–31
10. Freeman B. Screening for Atrial Fibrillation Using a Smartphone: Is There an App for That? Journal of the American Heart Association 2016; 5: e004000
11. App can detect irregular heart rhythm by looking at your face. http://news.heart.org/app-can-detect-irregular-heartbeat-by-looking-at-your-face/ (accessed 12th May 2017)
12. Hobbs FDR, et al. A randomised controlled trial and cost- effectiveness study of systematic screening (targeted and total population screening) versus routine practice for the detection of atrial fibrillation in people aged 65 and over. The SAFE study. Health Technology Assessment, 9, iii-iv, ix-x, 1-74
1. Lowres N, et al. Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. Thrombosis & Haemostasis 2014; 111: 1167–76
14. Svennberg E, Engdahl J, Al-Khalili F, et al. Mass screening for untreated atrial fibrillation: the STROKESTOP study. Ciculation 2015; 131: 2176–84
15. Gaillard N, Deltour S, Vilotijevic B, et al. Detection of paroxysmal atrial fibrillation with transtelephonic EKG in TIA or stroke patients. Neurology 2010; 74: 1666–70
16. Gladstone DJ, Bui E, Fang J, et al. Atrial Fibrillation in Patients with Cryptogenic Stroke. NEJM 2014; 370: 2467–77
17. Sanna T. Cryptogenic Stroke and Underlying Atrial Fibrillation. NEJM 2014; 370: 2478–86
18. Hariri E, et al. Optimal Duration of Monitoring for Atrial Fibrillation in Cryptogenic Stroke: A Nonsystematic Review. Biomed Research International 2016 – Article ID 5704963
19. Arsava EM, et al. Ischemic Stroke Phenotype in Patients With Nonsustained Atrial Fibrillation. Stroke 2015; 46: 634-40
20. Tran RT, et al. Short runs of atrial arrhythmia and stroke risk: a European-wide online survey among stroke physicians and cardiologists. Journal of the RCPE 2016; 465: 87-92
21. Healey JS, et al. ASSERT Investigators. Subclinical atrial fibrillation and the risk of stroke. NEJM 2012; 366: 120–129
22. Glotzer TV, et al. MOST Investigators. Atrial high rate episodes detected by pacemaker diagnostics predict death and stroke: report of the Atrial Diagnostics Ancillary Study of the MOde Selection Trial (MOST). Circulation 2003; 107: 1614–19
23. Glotzer TV, et al. The relationship between daily atrial tachyarrhythmia burden from implantable device diagnostics and stroke risk: the TRENDS study. Circulation Arrhythmia and Electrophysiology 2009; 2: 474–80



Comments are closed.