Pavilion Publishing and Media Ltd
Blue Sky Offices Shoreham, 25 Cecil Pashley Way, Shoreham-by-Sea, West Sussex, BN43 5FF, UNITED KINGDOM
The greatest risk from long-term overexposure to sunlight is thought to be skin cancer. Given the higher incidence in older patients, it is critical that this demographic is fully informed about the signs and symptoms that possibly indicate malignant changes.
Key learning objectives:
- What are the damaging effects of UV radiation?
- What are the signs and symptoms of the different types of skin cancer?
- How to diagnose and manage basal cell carcinoma
- How to diagnose and manage squamous cell carcinoma
- How to diagnose and manage melanoma
CPD credits: 0.5. Log them at myCPD
Introduction
For many of us, exposure to sunlight induces a sense of well-being, but a further and more important benefit, is the cutaneous production of vitamin D, mainly during the spring/summer months between the hours of 10am and 3pm.
Sunlight consists of roughly equal amounts of visible (400–700nm) and infrared (700–2,000m) radiation with approximately 10% ultraviolet radiation (100–400nm) and it this latter region that is responsible for the negative effects of sunlight.
UV radiation is subdivided into three bands:
- UVC (100–280nm)
- UVB (290–320nm)
- UVA (320–400nm)
As the energy of electromagnetic radiation is inversely proportional to the wavelength, UVC radiation, with the lowest wavelength range, is the most energetic and has the greatest potential to cause skin damage. Fortunately, UVC radiation is absorbed by the ozone layer and the remaining UV portion of the solar spectrum which passes through the atmosphere contains roughly 5% UVB and 95% UVA, both of which are potentially damaging to the skin. While UVB is the main cause of sunburn, both UVB and UVA are carcinogenic.
Damaging effects of UV radiation
Once UVB radiation hits the skin it is absorbed by DNA leading to the formation of two characteristic products. The first are known as cyclobutane pyrimidine dimers (CPDs), which are formed by covalently linking together two adjacent pyrimidine bases within the DNA (eg. cytosine and thymine).
The second type of products are 6,4 pyrimdine-pyrimidone photoproducts (6,4-PP) which are created when a bond is formed between the 6 and 4 carbon atoms in adjacent aromatic pyrimidine rings within DNA. These UVB-induced CPDs constitute the major signs of DNA damage (accounting for as much as 75%) with the remainder consisting of 6,4-PP. The generation of CPDs and 6,4-PPs are the hallmarks of UVB induced photo-damage in DNA and even sub-erythemal doses of UVB radiation can induce CPD and 6,4-PP in human skin.
UVA radiation can also exert deleterious effects on the skin through the generation of reactive oxygen species (ROS), which damage DNA and various cellular proteins and lipids. For example, production of 8-oxo-7-hydrodeoxyguanosine, an oxidized purine, is a recognised sign of oxidative damage, which may be important in mutagenesis. There is also evidence showing that UVA can induce CPDs and how these are removed at a much lower rate than the CPDs induced by UVB radiation.
The skins’ response to UV radiation
Although CPDs and 6,4-PP are markers of UV-induced skin damage, upon exposure to UV radiation, the skin increases the production of melanin, from melanocyte cells and this leads to tanning. Melanin consists of two different pigments: phaeomelanin, which is more prevalent in red haired individuals and creates a red to pink hue and eumelanin which is more prevalent in those with darker skins.
The melanin is produced in melanosomes and transported along dendritic projections to “cover” epidermal cells, shielding them from the effects of UV radiation. In addition, melanin acts to absorb UV radiation and also stimulates epidermal hyperplasia which serves to increase the radiation path in the skin and hence decrease penetration of UV radiation.
Despite these efforts to minimise the UV-induced damage, there are distinct markers of cumulative skin damage in the form of the pre-malignant cancers, actinic (i.e. caused by sunlight) keratoses (AKs) and Bowen’s disease, both of which have the potential to become dysplastic.
AKs are common in the older patient, affecting 19 and 24% of people over the age of 60 in the UK1 and most often seen in fair-skinned individuals originating as small, rough spots which are more easily felt than seen; a common analogy is that the affected area feels like sandpaper.
While it is possible to develop a single actinic keratosis lesion, it is more common for multiple lesions to develop in the same area of skin such as the scalp, a phenomenon referred to as a “field change”, i.e. the area of skin has extensive actinic damage.
Bowen’s disease arises in the outer layers of the epidermis with a peak incidence in the seventh decade and presents as a slow growing, hyperkeratotic patch or plaque with an irregular border though is sharply demarcated with a pink or red surface, sometimes with crusting that may grow to a few centimetres in size. Fortunately, the risk of malignant transformation is relatively low at around 3–5%.2
The different types of skin cancer: signs and symptoms
The greatest risk from long-term overexposure to sunlight is thought to be skin cancer. There are three forms of skin cancer: basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and melanoma with the former two often referred to as nonmelanoma skin cancers (NMSCs).
According to the latest information from Cancer Research UK, in 2015–2017, there were 16,202 cases of melanoma and 2,333 deaths.3
This equates to 44 new cases per day and it is the fifth most common cancer in the UK. Furthermore, the incidence of melanoma is age-related with 28% of cases occurring in people aged 75 years and over. In contrast to melanoma, the incidence of non-melanoma skin cancer is considerably higher with 151,739 cases recorded in the UK between 2015–2017 but only 1,115 deaths and on average, nearly half (47%) of all NMSCs occur in people aged 75 years and over.4
Basal cell carcinoma
Basal cell carcinomas (BCCs) arise, as the name suggests, from the basal layer of the epidermis and account for as much as 80% of all non-melanoma skin cancers. These tumours are commonly found on sun-exposed surfaces such as the head and neck and are slow growing and fortunately, rarely undergo metastasis but can cause extensive destruction of local tissue and lead to disfigurement.
Basal cell carcinomas are sometimes referred to as a “rodent ulcer”, derived from the fact that the lesion is locally invasive, effectively, “burrowing” in the skin.
The precise cause of BBC remains unclear although several epidemiological studies suggest a strong link with UV exposure5 as over 50% of BCCs show a defect in the p53 gene,6 which produces a tumour suppression protein. Nevertheless, the totality of the evidence remains inconclusive with a recent systematic review that examined the risk of occupational sun exposure on skin cancers, finding that only 11 of 19 studies reported statistically significant increased risks for a BCC.7
Since up to a fifth of BCCs occur on non-sun exposed part of the body, there are several other risk factors including a positive family history of the cancer, fair complexion, easy sunburning and immunosupression.8
Clinical symptoms of skin cancer
In the early stages, patients will often complain of a small, raised, slow growing lesion that bleeds and does not heal properly. Once developed, a BCC tends to have a raised border with a central ulcerated area.
Pulling the skin apart between two fingers will often highlight the border and closer inspection will usually reveal the presence of telangiectasias as seen in Figure 1.

There are four main forms of a BCC:
- Nodular—which is the most common type (roughly 60%) and tends to occur on the face
- Superficial—which are most common in younger patients
- Morphoeic— normally found at mid-face sites
- Basosquamous carcinoma—this is a mixed BCC and squamous cell carcinoma and is potentially the most aggressive form.
Management of skin cancer
The management is largely dependent upon factors including the lesion size and its location on the body. In a 2021 revision of guidance, the British Association of Dermatologists (BAD) have suggested that in most cases of a primary BCC, surgery, including standard excision, Mohs micrographic, curettage, cautery, cryotherapy and laser are the recommended treatment modality.9 Nevertheless, topical therapy with imiquimod and 5-fluorouracil are also available and licensed for the treatment of BCCs.
Preventative therapy
Non topical treatment options include cryotherapy and surgical excision. While sun protection measures such as sunscreens, are often recommended and despite limited evidence for effectiveness,10 the BAD guidance does suggest the use of this measure.
Squamous cell carcinoma
A squamous cell carcinoma (SCC) arises in the superficial layers of keratinocytes and unlike BCCs, can metastasize, in a small number of cases, particularly larger lesions. The incidence of SCC in the UK is slightly higher in men (56%) compared to women and the highest number of cases arise in people over the age of 90 years, reflecting greater cumulative UV exposure. Moreover, there is evidence that the incidence of SCC is increasing globally. with approximately 25,000 SCCs diagnosed each year.
The most common risk factor for the development of an SCC is chronic UV exposure and this no doubt explains why the incidence is higher in Caucasians. The condition is also two to three times more common in men than women and this gender difference is suggested to be due the greater tendency for men rather than women to have outdoor occupations and hence receive higher exposure to the sun. Immunocompromised patients are also at a much higher risk of developing SCC.
Clinical symptoms
A SCC will normally present as an indurated, nodular keratinising or crusted tumour which can ulcerate or appear as an ulcer without keratinisation.11 The carcinoma is typically found on sun-exposed areas, most frequently, the lower lip, external ear and periauricular region, forehead and scalp. It can also appear as a small nodule that enlarges and becomes necrotic in the central region that sloughs and develops into an ulcer.
An SCC may also appear as a slow-growing ulcer or reddish skin plaque. Patients who develop an SCC on the ear are at greatest risk of metastases.
Management
According to guidance from NICE, patients with suspected SCC should be referred to a specialist under the two-week cancer referral pathway.12 The most common treatment is surgical excision including a margin or normal surrounding skin. The updated BAD guideline states that there is insufficient evidence to support any recommendation for cryotherapy, CO2 laser or topical therapy in the treatment of SCC.11
Melanoma
The most serious form of skin cancer is a melanoma which arise from cancerous growth of the melanocytes in the basal layer of the epidermis. In contrast, non-cancerous growth leads to benign melanocytic naevi (i.e. moles), freckles and lentigines. While the majority of melanomas present in the skin, the condition can also arise in the eyes, oral cavity, lips and vagina.
The word melanoma comes from the Greek word “melas” which means black and the world-wide incidence of melanoma is increasing. The incidence of melanoma has more than doubled since the 1990s, although according to Cancer Research UK, over the last decade mortality has stabilised. Nevertheless, melanoma is an aggressive cancer and tends to metastasize and while in the early stages, treatment with surgery is effective, once advanced, surgical treatment is no longer possible and survival rates drop significantly.
Clinical symptoms
The symptoms of a melanoma vary depending on the type of which there are four.
1. Superficial spreading melanoma (SSM)
This is the most common type, accounting for 70% of cases and these tend to spread laterally on the surface of the skin rather than vertically towards the dermis. It is the most common type of melanoma seen in middle-aged patients. Initially, there is a flat or even slightly raised discoloured area of skin with irregular borders of varying colour. Some SSM arise in an existing mole, while others appear spontaneously. It is often seen on the legs of women and the trunk of men or on the upper back of both.
2. Nodular melanoma
These proliferate down into the skin and present as a nodule that has been rapidly enlarging over a period of a few weeks to months. As with a SSM, nodular melanomas can arise from an existing naevus or as a new lesion. Nodular melanoma more commonly appears on the head or neck.
3. Lentigo maligna
This is similar to type 1 (SSM) and presents as a flat or slightly elevated brown or dark brown discoloration in the skin that is frequently seen on exposed areas such as the face, ears, arms or upper trunk of older patients. A lentigo maligna is sometimes referred to as an in-situ melanoma and is slightly more common in women and is very slow growing. The rate of conversion of a lentigo maligna into a melanoma is lower than the other types and represents around 5% of all melanoma cases and is diagnosed when the lesion invades the dermis.
4. Acral lentiginous melanoma (ALM)
This type also spreads laterally before penetrating into the dermis. In contrast to the other forms of melanoma, an ALM appears initially as a black or brown lesion under the nails or on the soles of the feet or palms. The lesions start as a flat patch of discoloured skin. It is rarely seen in Caucasians (less than 1% of cases) but is the most common form in those with darker skin types, accounting for up to 72% of all melanoma cases. The cause is unknown since given its usual location; it is unlikely to be due to over-exposure to UV radiation.
Risk factors for melanoma
There are numerous proposed risk factors for melanoma which include:13
- Family history (2.2-fold higher risk)
- Personal characteristics such as blue eyes, fair/and or red hair, pale complexion
- Immunosuppressive states
- Atypical mole syndrome (i.e. high number of cutaneous moles)
An important contributory factor in the development of melanoma is exposure to sunlight and the use of sunbeds. In fact, a huge amount of laboratory, animal and observational studies have shown a significant and positive association between UV radiation and an increased risk of melanoma.14 However, it has been argued that since the reported association of sunbed use and melanoma is based on observational data (which is considered to be a low quality), there is little convincing evidence that sunbed use is casually related to melanoma.15
Recognition of melanomas
The differentiation between a benign melanocytic naevus and a melanoma can be difficult and it is best to refer all suspected cases to a dermatologist. However, a check-list has been developed which can assist primary care practitioners in the recognition of a melanoma, known as the ABCDE list as shown in Figure 2.
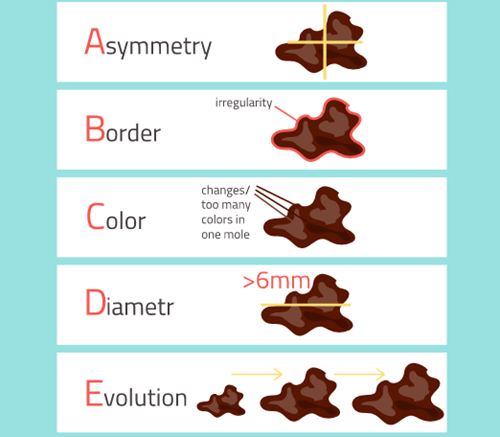
Asymmetry—in contrast to a benign naevus, a melanoma lesion is often non-symmetrical in shape, i.e., one half should be the mirror image of the other half, reflecting the uneven growth of the lesion.
Border—the edges of a melanoma is uneven.
Colour—normally naevi have a uniform colour whereas in a melanoma, there can be colour variation within the lesion.
Diameter—usually a melanoma is larger than a quarter of an inch (6 mm) although this is not always the case.
Elevation—although melanomas change in shape, size and colour, over time they become raised above the skin surface.
In addition to the ABCDE signs described above, NICE has identified a further 7-point checklist that healthcare professions should use when considering referring a patient with a suspected melanoma as shown in Table 1.
| Stage | Description |
| 0 | A melanoma in situ, i.e., it remains in the epidermis and has not spread into the dermis. |
| 1 | Melanoma no more than 2 mm thick and which has not spread |
| 1A | Melanomas |
| 1B | Melanomas |
| 2 | Usually thicker than stage 1 but still localized |
| 2A | Melanomas 1 – 2 mm thick with ulceration or 2 – 4 mm thick without ulceration |
| 2B | Melanoma 2 – 4 mm thick with or without ulceration |
| 2C | Melanoma thickness > 4 mm and ulcerated |
| 3 | Melanoma has spread to lymph nodes closest to melanoma but no further & divided into A, B and C depending on No lymph nodes involved |
| 4 | Melanoma cells have spread to other areas of the body, i.e., has metastasized.
*Note that melanomas which are ulcerated are more likely to spread |
Table 1. Different melanoma stages16
All patients scoring 3 or more on this checklist should be referred under the 2-week cancer referral pathway.
Management of skin cancer
The treatment of melanoma depends on the extent to which it has spread which is referred to as “staging” as described in the Table 1 and illustrated in Figure 3.
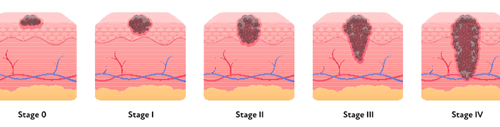
Treating stages 0, 1 and 2 melanomas
Stage 0, 1 and 2 melanomas are surgically removed, usually under local anaesthetic and the excision margin depends on the stage. For instance, a stage 0 melanoma requires a 0.5 cm margin, stage 1 a 1 cm margin and 2 cm for stage 2.
Stage 3 management
A stage 3 melanoma is normally diagnosed after a sentinel node biopsy and requires completion lymphadenectomy since a sentinel node biopsy will have confirmed micro-metastases.
Stage 4 management
Immunotherapy is often used for metastatic melanoma and such treatments stimulates the body’s own immune system to attack cancer cells. Two drugs nivolumab and ipilimumab are used in the management of advanced melanoma. Nivolumab targets the protein PD-1 which normally prevents T cells from recognising and attacking cancer cells. By blocking the interaction of PD-1 between tumour and T -cells, nivolumab is able to prevent the tumour cells from evading the immune system.
Ipilimumab targets the CTLA-4 protein, a second protein which prevents cytotoxic T lymphocytes from killing cancer cells. The combination of nivolumab and ipilimumab has been advocated by NICE for the treatment of advanced melanoma.17
Conclusion
In summary, skin cancer causes considerably morbidity and mortality and is more prevalent with advancing years. The provision of safe sun advice such as avoiding spending time in direct sunlight between the hours of 10am and 3pm, wearing sunglasses, hats, protective clothing and sunscreens, are measures which can be easily implemented.
Given the higher incidence in older patients, it is critical that this demographic is fully informed about the signs and symptoms that possibly indicate malignant changes in an attempt to ensure early and more importantly, potentially saving lives.
Rod Tucker is a pharmacist researcher with an interest in dermatology
Conflict of interest: none declared.
References
- de Berker D, McGregor JM, Mohd Mustapa MF, Exton LS, Hughes BR. British Association of Dermatologists’ guidelines for the care of patients with actinic keratosis 2017. Br J Dermatol 2017; 176(1): 20-43
- Morton CA, Birnie AJ, Eedy DJ. British Association of Dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen’s disease) 2014. Br J Dermatol 2014; 170(2): 245–60
- UK CR. Melanoma skin cancer statistics 2021 Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/melanoma-skin-cancer Accessed 05/07/21
- Non-melanoma skin cancer incidence statistics 2021 Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/non-melanoma-skin-cancer/incidence. Accessed 05/07/21
- Marzuka AG BS. Basal Cell Carcinoma: Pathogenesis, Epidemiology, Clinical Features, Diagnosis, Histopathology, and Management. Yale J Bio Med 2015; 88: 167–79
- Rady P SF, Wagner RF et al. p53 mutations in basal cell carcinomas. Cancer Res 1992; 52(13): 3804–6
- Loney T, Paulo MS, Modenese A, et al. Global evidence on occupational sun exposure and keratinocyte cancers: a systematic review. Br J Dermatol 2021; 184(2): 208-18
- McDaniel B BT, Steele RB. Basal cell carcinoma 2020 Available from: https://www.ncbi.nlm.nih.gov/books/NBK482439/. Accessed 05/07/21
- Nasr I, McGrath EJ, Harwood CA, Botting J, Buckley P, Budny PG, et al. British Association of Dermatologists guidelines for the management of adults with basal cell carcinoma 2021. Br J Dermatol 2021
- Sanchez G, Nova J, Rodriguez-Hernandez AE, et al. Sun protection for preventing basal cell and squamous cell skin cancers. Cochrane Database Syst Rev 2016; 7: CD011161
- Keohane SG, Botting J, Budny PG, et al. British Association of Dermatologists guidelines for the management of people with cutaneous squamous cell carcinoma 2020. Br J Dermatol 2021; 184(3): 401-14
- NICE. Suspected cancer: recognition and referral (NG12) 2015 (updated 2021) Available from: https://www.nice.org.uk/guidance/ng12/chapter/1-Recommendations-organised-by-site-of-cancer#skin-cancers. Accessed 05/07/21
- Heistein JB AU. Malignant melanoma StatPearls2020 Available from: https://www.ncbi.nlm.nih.gov/books/NBK470409/. Accessed 05/07/21
- Raimondi S, Suppa M, Gandini S. Melanoma Epidemiology and Sun Exposure. Acta Derm Venereol 2020; 100(11): adv00136.
- Burgard B, Schope J, Holzschuh I, et al. Solarium Use and Risk for Malignant Melanoma: Meta-analysis and Evidence-based Medicine Systematic Review. Anticancer Res. 2018; 38(2): 1187-99
- Stages of melanoma 2018 Available from: https://www.melanomauk.org.uk/stages-of-melanoma. Accessed 05/07/21
- NICE. Nivolumab in combination with ipilimumab for treating advanced melanoma (TA 400) 2016 Available from: https://www.nice.org.uk/guidance/ta400 Accessed 05/07/21


